Publication History
Submitted: February 19, 2025
Accepted: March 02, 2025
Published: April 30, 2025
Identification
D-0419
DOI
https://doi.org/10.71017/djmi.4.4.d-0419
Citation
Bikramaditya Prasad Sah (2025). Outcome Comparison in Microscopic and Endoscopic Trans-Sphenoidal Pituitary Adenoma Surgery in Terms of Extent of Resection. Dinkum Journal of Medical Innovations, 4(04):165-176.
Copyright
© 2025 The Author(s).
165-176
Outcome Comparison in Microscopic and Endoscopic Trans-Sphenoidal Pituitary Adenoma Surgery in Terms of Extent of ResectionOriginal Article
Bikramaditya Prasad Sah 1*
- Consultant Neurosurgeon, Lahore General Hospital Neurosurgery Unit III, Lahore, Pakistan.
* Correspondence: psbikramaditya@gmail.com
Abstract: The current standard interventions for pituitary adenomas are transsphenoidal surgery by endoscopic or microscopic approaches. However, the superiority of efficacy and safety of the two surgical procedures remain controversial. This study compared the outcome of endoscopic and microscopic transsphenoidal pituitary adenoma surgery by randomized controlled trial method. It is done in Department of Neurosurgery, Lahore General Hospital, Lahore for a period of 12 months. Total N=60 patients were enrolled, patients were randomly divided in two groups by using lottery method. In group A, patients undergone transsphenoidal pituitary adenoma surgery through endoscopic approach while in group B, patients undergone transsphenoidal pituitary adenoma surgery through microscopic approach. During and after surgery CSF leakage and resection in terms of gross total, subtotal and partial were noted. Patients were followed-up in OPD. At 6 weeks, visual field of patients were assessed and improvement was noted. A predesigned proforma was used to collect information. Visual field improvement was slightly higher in patients who were operated via microscopic approach as compared to those with endoscopic approach but the difference in both the groups is insignificant i.e. Group-A: 95.7% vs. Group-B: 96% (p-value>0.05). Regarding CSF leak, the difference was observed was insignificant in both treatment groups i.e. Group-A: 13.3% vs. Group-B: 16.7% (p-value>0.05). Gross total resection (GTR) was seen in 73.3% and subtotal resection (STR) in 26.7% patients who were operated with endoscopic approach while patients who were operated with microscopic approach, GTR was in 66.7% and STR in 33.3% patients (p>0.05) which is insignificant. Both treatment modalities are nearly equally effective in treating pituitary adenoma. Although with endoscopic approach comes up with higher gross total resection of pituitary adenoma.
Keywords: endoscopic, microscopic, transsphenoidal, pituitary, adenoma
- INTRODUCTION
The incidence of pituitary tumors is found in 10 to 15% among all intracranial tumors. Incidental pituitary tumors are found in approximately 10% of autopsies [1]. Pituitary adenoma occurs in anterior lobe of pituitary gland. Pituitary tumors are classified on the basis of size and hormonal activity. Pituitary adenomas with size less than 10mm and ≥10mm are microadenomas and macroadenomas respectively. While hormonally active and inactive adenomas are known as functional and non-functional type respectively. The estimated prevalence rate of pituitary adenomas is around 17% [2]. Improvement in different treatment modalities e.g. medical, surgical as well as hormonal replacement therapies have led to better outcome with low mortality rate [3]. However, maximum appropriate delivery of services, distribution of resources and latest advanced diagnostic technologies according to impact of these tumors in the community are needed for their early diagnosis and management [4]. Surgery is commonly used in the management of pituitary adenomas [5]. Different complications such as irreversible visual impairment, ophthalmoplegia and other neurological complications of macroadenomas are associated with morbidity; and pituitary apoplexy is the life-threatening complication [6]. Horsley was the first who reported the open craniotomy through which pituitary tumor surgeries were performed. While [7] described pituitary adenoma surgery through transsphenoidal approach. An author [8] brought the sublabial transseptal transsphenoidal approach into the practice and avoided using external incision and this was associated with least morbidity and mortality. An author [9] used surgical microscope and intraoperative radiological visualization; and popularized Cushing’s technique. This microscope has advantages of stereoscopic view. An author [10] used fully endoscopic endonasal approach for removal of pituitary lesion. This endoscopic approach has advantages of having panoramic view inside sphenoid sinus and pituitary fossa i.e. Sella turcica, better visualization and less invasiveness which gives direct access to innermost skull base lesion. However, the endoscope has the disadvantage of lacking the stereoscopic view, which makes both endoscopic and microscopic transsphenoidal approaches equivocal in pituitary adenoma operation [11]. The trans-sphenoidal approach has been proposed as a minimally invasive surgical technique for the removal of pituitary tumors [12]. Microscopic trans-sphenoidal approach for pituitary tumor surgery remains the benchmark for future surgical techniques. In recent year, endoscopic endonasal approach is more preferred than microscopic approach. Endoscopic endonasal approach gives favourable outcome as compared to microscopic approach in terms of extent of tumor resection and control of functional pituitary tumor [12]. Cushing’s disease can be safely and effectively treated via endoscopic transsphenoidal approach. But recurrence rates remain comparable in both endoscopic and microscopic transsphenoidal approaches [13]. Resection of pituitary adenoma via endoscopic transsphenoidal approach has become more popular but is associated with higher rate of vascular injury in comparison to microscopic transsphenoidal pituitary adenoma surgery. Microscopic transsphenoidal resection of pituitary adenoma is widely and well-established approach with favourable outcome [14]. In a randomized trial, it was observed that the endoscopic and microscopic approach had GTR 81.7% versus 62.2%, (P < 0.05) respectively. However, the incidence of CSF rhinorrhea between endoscopic and microscopic groups (P > 0.05) are similar. Endoscopic approach has advantages of wide operative field and makes easier to differentiate the tumor tissues from normal tissues and surrounding structures by giving broad lateral vision even in the corner of the Sella turcica. According to above study, Pituitary adenoma surgery via endoscopic approach is safe and has better short-term outcome as compared to microscopic approach [15]. Another trial conducted on 25 patients in microscopic group and 25 patients in endoscopic group for resection. In the microscopically treated group, there were 24% CSF leaks and 77% patients had gross total resection on postoperative imaging. In endoscopically treated group, 28% had CSF leaks and 66% patients had gross total resection. There was insignificant difference in both groups and authors concluded that endoscopic procedure has almost similar outcome as with microscopic procedure [16]. One trial showed that with microscopically treated cohort, there were complete resection in 60% patients, subtotal in 36% cases and 4% patients had partial resection. In endoscopically treated group, there were complete resection in 73.17% patients, subtotal in 23.17% cases and 3.65% patients had partial resection. There was insignificant difference in both groups (P>0.05) [17]. Regarding visual improvement, it was stated that the difference in the rates of visual improvement in both i.e. endoscopic approach and microscopic approach is not significant. (P > 0.05) [18]. So, rationale of this research is to compare the outcome of endoscopic and microscopic transsphenoidal pituitary adenoma surgery in terms of extent of resection, visual field improvement and CSF leakage. In literature, it has been reported that endoscopic approach is more successful and effective in removing pituitary adenoma as compared to microscopic approach. Although microscopic approach is still in use. Because of unavailability of local evidence on this regard, this study is being performed whether endoscopic or microscopic approach is better for local population. This helped to improve our practice as well as if proved through this study that endoscopic approach is better, then in future we will try to implement the use of endoscopic approach instead of microscopic approach transsphenoidal pituitary adenoma surgery. Pituitary adenomas usually affect individuals with median age of 37 years and more commonly affect female than male while Non-functional subtype predominantly affects male. The diagnostic delay was longer for acromegaly. Awareness of these treatable conditions minimize the adverse sequelae of delayed diagnosis [19]. The pituitary microadenomas like incidentalomas have unrecognized impact on fertility and quality of life for long duration [19]. Pituitary adenomas commonly causing hypopituitarism are macroadenomas, of which most of them are non-functioning adenomas [20]. The pituitary gland releases different types of hormones into the circulation which control most of endocrine system of body. The pituitary gland is found in Sella turcica of sphenoid bone and is isolated from brain above by arachnoid mater and diaphragm Sella [21]. The pituitary gland consists of two different lobes i.e. the anterior lobe and the posterior lobe divided by the par’s intermedia [22]. The posterior lobe contains axons of neurons that extend from the hypothalamus to which it is connected via the pituitary stalk. The antidiuretic hormone and oxytocin produced by the neurons of the supraoptic and paraventricular nuclei of the hypothalamus released from axonal endings within the posterior lobe of pituitary gland [22]. The anterior lobe of pituitary gland produces different types of hormones such as TSH, ACTH, FSH, LH, GH and prolactin. The pathology in the pituitary gland was reported by Pierre, a French neurologist. Initially while Harvey Cushing and Sir Arthur Keith in 1909 reported an increased size of Sella turcica in the patients with pituitary tumor [23]. this study compared the outcome of endoscopic and microscopic transsphenoidal pituitary adenoma surgery.
- MATERIALS & METHOD
It is a Randomized Controlled Trial study which is performed in Department of Neurosurgery, Lahore General Hospital, Lahore for a period of 12 months after submission of synopsis. Sample size of 94 cases; 47 cases in each group are calculated with 80% power of test, 10% level of significance and taking expected percentage of gross tumor removal i.e. 81.7% with endoscopic approach and 62.2% with microscopic approach by using following formula [24].
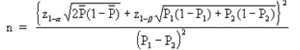
Were,
Z1-α = 90% confidence interval (as α=10%) = 1.65
Z1-β = 80% power of test = 1.282
P1 = proportion of sample 1 = 0.817
P2 = proportion of sample 2 = 0.622
P(bar) = difference in both proportions = 0.195
But Sample size of 60 cases; 30 cases in each group were taken because of limited duration of study, availability of cases and surgeries in a year. Non-Probability, Consecutive sampling technique was used. 60 patients fulfilling inclusion criteria were enrolled from wards of department of Neurosurgery, Lahore General Hospital, Lahore. Informed consents were obtained. Demographic variables (name, age, gender and duration of symptoms of pituitary adenoma) were noted. Proper history and neurological examination were carried out. Routine blood investigations were done. Then patients were randomly divided in two groups by using lottery method. In group A, patients underwent transsphenoidal pituitary adenoma surgery through endoscopic approach while in group B, patients underwent transsphenoidal pituitary adenoma surgery through microscopic approach. During and/or after surgery CSF leakage was noted. Post-operatively, patients were shifted in ICU or post-operative ward and then ward. Patients were followed-up in OPD (outpatient department) till 6 weeks of procedure and visual fields were assessed by confrontation method and were noted. Extent of resection was noted. A predesigned proforma was used to collect information (attached). The collected data were entered and analyzed by using SPSS version 21. The study results were analyzed in an intention to treat population, as all patients had to follow the study protocol at time of randomization. Quantitative variables like age, duration of symptoms of pituitary adenoma were presented as mean and SD. Qualitative variables like gender, gross total resection, subtotal resection, partial resection, CSF leak and visual field improvement were presented as frequency and percentage. Chi-square was applied to compare frequency of gross total resection, subtotal resection, partial resection, CSF leak and visual field improvement in both groups. P-value≤0.05 was taken as significant. Data was stratified for age, gender and duration of symptoms of pituitary adenoma.
- RESULTS & DISCUSSION
Mean age of patients in Group-A & in Group-B were 38.63±14.16 and 42.40±10.16 years respectively. Table 01. In Group-A 19(63.3%) patients were male and 11(36.7%) were female. While in Group-B 18(60%) patients were male and 12(40%) were female respectively. Table 02. Mean duration of symptoms for patients in Group-A and in Group-B were 20.47±31.55 months and 14.22±19.49 months respectively. Table 03. At baseline visual field, visual impairment was in 23 patients in Group-A while in 25 patients in Group-B. Table 04. Improvement in visual field was higher in Group-B patients as compared to Group-A patients. i.e. Group-A: 95.7% vs. Group-B: 96.0%, although it is insignificant (p-value>0.05). Table 05. In Group-A, patient’s gross total resection was done in 22(73.3%) patients and subtotal resection was done in 8(26.7%) patients while in Group-B, gross total resection was done in 20(66.7%) patients and subtotal resection was done in 10(33.3%) patients. Partial resection was not seen in any case in either group. The difference in extent of resection in each group was insignificant (p>0.05). Table 06. In Group-A, 4(13.3%) patients and in Group-B 5(16.7%) patients had CSF leak. In both treatment groups no significant difference was seen for CSF leak (p-value>0.05) Table 07. Visual field improvements in both treatment groups were compared through stratification of age, gender and duration of pituitary adenoma to see the effect of these variables in both treatment groups. Details can be seen in Table 08, 09 & 10. Effects of age, gender and duration of pituitary adenoma on resection in both treatment groups are given in Table-11, 12 & 13. Except age, gender and duration of pituitary adenoma, there was no significant impact on CSF leak in both treatment groups. Details can be seen in Table-14, 15 & 16
Table 01: Age of patients in treatment groups
| Group-A | Group-B | |
| N | 30 | 30 |
| Mean | 38.63 | 42.40 |
| SD | 14.16 | 10.16 |
| Min | 20 | 20 |
| Max | 65 | 65 |
Group-A: Endoscopic approach
Group-B: Microscopic approach
Table 02: Gender of patients in treatment groups
| Group-A | Group-B | Total | |
| Male | 19(63.3%) | 18(60%) | 37 |
| Female | 11(36.7%) | 12(40%) | 23 |
| Total | 30 | 30 | 60 |
Group-A: Endoscopic approach
Group-B: Microscopic approach
Table 03: Descriptive statistics for duration of symptoms (months)
| Group-A | Group-B | |
| N | 30 | 30 |
| Mean | 20.47 | 14.22 |
| SD | 31.55 | 19.49 |
| Min | 1 | 1 |
| Max | 96 | 75 |
Group-A: Endoscopic approach
Group-B: Microscopic approach
Table 04: Baseline visual field
| Group-A | Group-B | Total | ||||
| Normal vision | 7 | 5 | 12 | |||
| Visual impairment | 23 | 25 | 48 | |||
| Total | 30 | 30 | 60 | |||
| Visual impairment | ||||||
| Bi temporal hemianopia | 13 | 9 | 22 | |||
| Left blind /Right light perception | 1 | 0 | 1 | |||
| Left blind /Right temporal hemianopia | 1 | 0 | 1 | |||
| Left hand movement perception/Right temporal hemianopia | 6 | 6 | 12 | |||
| Left temporal hemianopia/ Right normal | 0 | 2 | 2 | |||
| Left normal/Right hand movement perception | 1 | 1 | 2 | |||
| Right hand movement perception/Left temporal hemianopia | 0 | 4 | 4 | |||
| Left normal/ Right temporal hemianopia/ | 1 | 1 | 2 | |||
| Right temporal hemianopia / Left light perception | 0 | 2 | 2 | |||
| Total | 23 | 25 | 48 | |||
Group-A: Endoscopic approach
Group-B: Microscopic approach
Table 05: Improvement in visual field at 6 weeks
| Visual Field | Group-A | Group-B | Total |
| Yes | 22(95.7%) | 24(96.0%) | 46 |
| No | 1(4.3%) | 1(4.0%) | 2 |
| Total | 23 | 25 | 48 |
Group-A: Endoscopic approach
Group-B: Microscopic approach
Chi-Square Test= 0.004
p-value= 0.952 (Insignificant)
Table 06: Resection in treatment groups
| Group-A | Group-B | Total | |
| GTR | 22(73.3%) | 20(66.7%) | 42 |
| SR | 8(26.7%) | 10(33.3%) | 18 |
| PR | 0 | 0 | 0 |
| Total | 30 | 30 | 60 |
Group-A: Endoscopic approach
Group-B: Microscopic approach
Chi-Square Test= 0.317
p-value= 0.573 (Insignificant)
Table 07: CSF Leak in treatment groups
| Group-A | Group-B | Total | |
| Yes | 4(13.3%) | 5(16.7%) | 9 (15.0%) |
| No | 26(86.7%) | 25(83.3%) | 51 (85.0%) |
| Total | 30 | 30 | 60 |
Group-A: Endoscopic approach
Group-B: Microscopic approach
Chi-Square Test= 0.131
p-value= 0.718 (Insignificant)
Table 08: Visual field improvement in treatment groups stratified for Age
| 20-35 Years | 36-50 Years | 51-65 Years | ||||
| Group-A | Group-B | Group-A | Group-B | Group-A | Group-B | |
| Yes | 14(100%) | 4(100%) | 5(83.3%) | 20(95.2%) | 3(100%) | 0(0%) |
| No | 0(0%) | 0(0%) | 1(16.7%) | 1(4.8%) | 0(0%) | 0(0%) |
| p-value | – | 0.326 | NA | |||
Table 09: Visual field improvement in treatment groups stratified for Gender
| Male | Female | |||
| Group-A | Group-B | Group-A | Group-B | |
| Yes | 16(94.1%) | 14(93.3%) | 6(100%) | 10(100%) |
| No | 1(5.9%) | 1(6.7%) | 0(0%) | 0(0%) |
| p-value | 0.927 | – | ||
Table 10: Visual field improvement in treatment groups stratified for Duration of pituitary adenoma
|
|
1-20 months | 21-40 months | 41-60 months | >60 months | ||||
| Group-A | Group-B | Group-A | Group-B | Group-A | Group-B | Group-A | Group-B | |
| Yes | 15(93.8%) | 18(94.7%) | 1(100%) | 3(100%) | 1(100%) | 2(100%) | 5(100%) | 1(100%) |
| No | 1(6.3%) | 1(5.3%) | 0(0%) | 0(0%) | 0(0%) | 0(0%) | 0(0%) | 0(0%) |
| p-value | 0.900 | – | – | – | ||||
Group-A: Endoscopic approach
Group-B: Microscopic approach
Table 11: Tumor resection in treatment groups stratified for Age
| 20-35 Years | 36-50 Years | 51-65 Years | ||||
| Resection | Group-A | Group-B | Group-A | Group-B | Group-A | Group-B |
| GTR | 15(88.2%) | 5(100%) | 4(50%) | 15(62.5%) | 3(60%) | 0(0%) |
| STR | 2(11.8%) | 0(0%) | 4(50%) | 9(37.5%) | 2(40%) | 1(100%) |
| PR | 0(0%) | 0(0%) | 0(0%) | 0(0%) | 0(0%) | 0(0%) |
| p-value | 0.421 | 0.533 | 0.273 | |||
Group-A: Endoscopic approach
Group-B: Microscopic approach
Table 12: Tumor resection in treatment groups stratified for Gender
| Male | Female | |||
| Resection | Group-A | Group-B | Group-A | Group-B |
| Gross Total | 14(73.7%) | 10(55.6%) | 8(72.7%) | 10(83.3%) |
| Subtotal | 5(26.3%) | 8(44.4%) | 3(27.3%) | 2(16.7%) |
| PR | 0(%) | 0(%) | 0(%) | 0(%) |
| p-value | 0.248 | 0.538 | ||
Group-A: Endoscopic approach
Group-B: Microscopic approach
Table 13: Tumor resection in treatment groups stratified for Duration of pituitary adenoma
| 1-20 months | 21-40 months | 41-60 months | >60 months | |||||
| Group-A | Group-B | Group-A | Group-B | Group-A | Group-B | Group-A | Group-B | |
| GTR | 18(81.8%) | 17(73.9%) | 0(0.0%) | 1(33.3%) | 1(100%) | 2(66.7%) | 3(50%) | 0(0.0%) |
| STR | 4(18.2%) | 6(26.1%) | 1(100%) | 2(66.7%) | 0(0.0%) | 1(33.3%) | 3(50%) | 1(100%) |
| PR | 0(0.0%) | 0(0.0%) | 0(0.0%) | 0(0.0%) | 0(0.0%) | 0(0.0%) | 0(0.0%) | 0(0.0%) |
| p-value | 0. 524 | 0.505 | 0.505 | 0.350 | ||||
Group-A: Endoscopic approach
Group-B: Microscopic approach
Table 14: CSF leakage in treatment groups stratified for Age
| 20-35 Years | 36-50 Years | 51-65 Years | ||||
| Group-A | Group-B | Group-A | Group-B | Group-A | Group-B | |
| Yes | 2(11.8%) | 0 (0.0%) | 1(12.5%) | 5(20.8%) | 1(20.0%) | 0(0.0%) |
| No | 15(88.2%) | 5 (100%) | 7(87.5%) | 19(79.2%) | 4(80.0) | 1(100%) |
| p-value | 0.421 | 0.601 | 0.624 | |||
Group-A: Endoscopic approach
Group-B: Microscopic approach
Table 15: CSF leakage in treatment groups stratified for Gender
| Male | Female | |||
| Group-A | Group-B | Group-A | Group-B | |
| Yes | 3(15.8%) | 2(11.1%) | 1(9.1%) | 3(25%) |
| No | 16(84.2%) | 16(88.9%) | 10(90.9%) | 9(75.0%) |
| p-value | 0.677 | 0.315 | ||
Group-A: Endoscopic approach
Group-B: Microscopic approach
Table 16: CSF leakage in treatment groups stratified for Duration of pituitary adenoma
|
|
1-20 | 21-40 | 41-60 | >60 | ||||
| Group-A | Group-B | Group-A | Group-B | Group-A | Group-B | Group-A | Group-B | |
| Yes | 1(4.5%) | 4(17.4%) | 1(100%) | 1(33.3%) | 0(0.0%) | 0(0.0%) | 2(33.3%) | 0(0.0%) |
| No | 21(95.5%) | 19(82.6%) | 0(0.0%) | 2(66.7%) | 1(100%) | 3(100%) | 4(66.7%) | 1(100%) |
| p-value | 0.170 | 0.248 | NA | 0.495 | ||||
Group-A: Endoscopic approach
Group-B: Microscopic approach
Endoscopy expands the limits of the surgeons’ performance of transsphenoidal surgery by improving visualization that they could not have accessed before. The characteristic of minimal invasiveness explains the positive outcomes and decreases post-operative complications rate via endoscopic approach in comparison with the microscopic one. Results of this study showed that visual field improvement was nearly equal in both approaches i.e. Group-A: 95.7% vs. Group-B: 96%, but the difference is insignificant (p-value>0.05). Studies have shown no significant difference regarding visual improvement for both treatment modalities. Mahmoud Messerer in his study showed improved visual outcome as 51% with endoscopic approach and 50% with microscopic approach [25]. An author in his study reported the recovery of visual function as 91.7% with Endoscopic endonasal transsphenoidal surgery [26]. A study reported improved visual function in patients as 86% who underwent endoscopic endonasal trans-sphenoidal surgery of pituitary macroadenomas [27]. however, in our study the difference in the rate of improvement in visual field with endoscopic and microscopic approaches are insignificant and is in line with the above-mentioned studies. Regarding CSF leak, no significant difference was seen in both groups i.e. Group-A: 13.3% vs. Group-B: 16.7% (p-value=0.131). Similar findings were reported by [28], (Endoscopic-Op: 12.1% vs. Microscopic Op: 8.5%, p-value=0.33), [29] (Endoscopic-Op: 15.38% vs. Microscopic Op: 11.76%, p-value=0.937), [30] and a recent meta-analysis reported the similar findings regarding no significant difference for CSF leak for both treatment modalities [31,32]. In this study, gross total resection was done in 73.3% and subtotal resection in 26.7% patients who were operated with endoscopic approach while patients who were operated with microscopic approach, among them gross resection was achieved in 66.7% and subtotal resection in 33.3% patients. Although with endoscopic approach, gross resection rate was higher but still it is not statistically significant (p>0.05). an author showed that with microscopically treated cohort, the complete, subtotal and partial resection were achieved in 60%, 36%, 4% patients respectively. While in endoscopically treated group, complete resection was achieved in 73.17% patients, subtotal in 23.17% cases and 3.65% patients had partial resection. There was insignificant difference in both groups (P>0.05) [33]. Authors showed higher rate of tumor resection in patients who underwent endoscopic approach as compared to microscopic approach. Result of this study regarding resection of tumor is in line with the results reported by above mentioned authors [34,35]. An author concluded that quality of resection is significantly improved after one year in those who were operated via endoscopic approach (GTR: 74% vs 50%, p=0.002) [36]. A study showed that trans-sphenoidal surgery with endoscope has better results in both tumor resection and control of disease in comparison with microscopic approach [22]. A study showed that the rate of control of disease is better when resection was done via endoscopic approach in comparison to the microscopic approach [37]. A study showed that endoscopic approach is better than the microscopic surgery in macroadenomas and adenomas with extension above the Sella because it helps to gain access and control over the para seller extension of the tumor. In addition, a previous pituitary or sinus surgery and the flap that might affect the intervention should be stratified in future studies [38]. Pituitary surgery via endoscopic trans-sphenoidal approach is a growing technique and comparison between microscopic and endoscopic surgery should be performed to evaluate merits and demerits. Operating microscope does not visualize whole of the sphenoid sinus, Sella turcica and surrounding structures. The endoscopic approach had a widened operative field of view, eliminates the need of a nasal speculum as guide and makes easier to differentiate of tumor tissues from gland. Endoscopic surgery had minimal damage to nasal cavity, minimize postoperative morbidity and with angled endoscope all area of nose and para-nasal sinus can be completely visualized. Optical properties of endoscope are better than the operating microscope. Endoscope gives an exquisite view of optic bulge, carotid bulge and optic carotid recess which reduces the chances of disastrous injury to internal carotid artery [38]. In our study, the mean duration of symptoms for patients in Group-A and in Group-B were 20.47±31.55 months and 14.22±19.49 months respectively. It was observed that around 75% cases presented within 12months of symptoms, while remaining 25% patients presented in 3-8 years (36-96months) of appearance of symptoms. Thus, there was presence of extreme values in data, so we got larger standard deviation than mean. This may because, patients of prolactinoma intolerance to medication and nonfunctional adenomas presented within 1-12 months of symptoms while patients of other types of pituitary adenomas presented between 36-96 months of symptoms. There are several limitations of endoscopic approach as it requires a bloodless surgical field and had a steep learning curve. In endo-nasal endoscopic surgery, there is no need of sublabial or nasal incision and elevation of mucoperichondrial flap from nasal septum. Hence, the possible complications of septal and para nasal sinus areas are eliminated.
- CONCLUSIONS
The present study highlights that the current standard interventions for pituitary adenomas, including endoscopic and microscopic transsphenoidal surgery, demonstrate comparable outcomes in terms of efficacy and safety. A randomized controlled trial was conducted in the Department of Neurosurgery, Lahore General Hospital, Lahore, over a period of 12 months, in which 60 patients were enrolled and randomly allocated into two groups. Patients in Group A underwent surgery using the endoscopic approach, whereas patients in Group B underwent surgery using the microscopic approach. Outcomes including cerebrospinal fluid (CSF) leakage, extent of tumor resection (gross total, subtotal, or partial), and postoperative visual field improvement were assessed using a structured proforma. At six weeks of follow-up, visual field improvement was slightly higher in the microscopic group compared to the endoscopic group (Group A: 95.7% vs. Group B: 96%), although this difference was statistically insignificant (p > 0.05). Similarly, the incidence of CSF leakage did not differ significantly between the groups (Group A: 13.3% vs. Group B: 16.7%, p > 0.05). Gross total resection was achieved in 73.3% of patients in the endoscopic group compared to 66.7% in the microscopic group, while subtotal resection was noted in 26.7% and 33.3% of patients, respectively, with no significant difference (p > 0.05). Overall, both surgical approaches were nearly equivalent in managing pituitary adenomas, although the endoscopic technique demonstrated a trend toward higher gross total resection rates. Importantly, no significant differences were observed between the two modalities regarding visual field recovery or CSF leakage. These findings suggest that both the endoscopic and microscopic transsphenoidal approaches remain viable and effective treatment strategies, each with its own advantages and limitations. Nevertheless, considering the limited sample size and single-center nature of this study, larger multicenter randomized controlled trials with longer follow-up are recommended to better define the comparative efficacy and to resolve the ongoing controversy over the preferred surgical approach for pituitary adenoma management.
REFERENCES
- Matharu, M.; Levy, M.; Merry, R. & Goadsby, P. 2003. Sunct Syndrome Secondary To Prolactinoma. Journal Of Neurology, Neurosurgery & Psychiatry, 74, 1590-1592.
- 2018. Cavernous Sinus And Its Cranial Nerves
- Eördögh, M., Bárány, L., Rosenstengel, C., Bogaczyk, V., Baldauf, J., Vogelgesang, S., … & Schroeder, H. W. (2025). Comparison of endoscopic and endoscope-assisted microscopic transsphenoidal surgery for pituitary adenoma resection: a prospective randomized study. Frontiers in Endocrinology, 16, 1552526.
- Zahidur Rahman Khan & Dr. Sabrina Tymee (2024). Evaluation of Prognostic Role of Serum CRP in Acute Stroke Patients. Dinkum Journal of Medical Innovations, 3(06):460-468.
- Ammirati, M.; Wei, L. & Ciric, I. 2012. Short-Term Outcome Of Endoscopic Versus Microscopic Pituitary Adenoma Surgery: A Systematic Review And Meta-Analysis. Journal Of Neurology, Neurosurgery & Psychiatry, Jnnp-2012-303194.
- Pala, A., Grübel, N., Mayer, B., Becker, R., Sommer, F., Schmitz, B., … & Hlavac, M. (2025). Endocrine Outcome and Quality of Life After Transsphenoidal Resection of Pituitary Adenoma—A Prospective Randomized Single-Blinded Study Comparing Endoscopic Versus Microscopic Resection. Neurology International, 17(1), 5.
- Asa, S. L. 2008. Practical Pituitary Pathology: What Does The Pathologist Need To Know? Archives Of Pathology & Laboratory Medicine, 132, 1231-1240.
- Asa, S. L. & Ezzat, S. 1998. The Cytogenesis And Pathogenesis Of Pituitary Adenomas 1. Endocrine Reviews, 19, 798-827.
- Asa, S. L.; Kovacs, K. & Bilbao, J. M. 1982. The Pars Tuberalis Of The Human Pituitary. Virchows Archiv A, 399, 49-59.
- Barnes, L.; Organization, W. H. & Cancer, I. A. F. R. O. 2005. Pathology And Genetics Of Head And Neck Tumours, World Health Organization.
- Basicmedical Key. 2016. Acromegaly
- Biousse, V.; Newman, N. & Oyesiku, N. 2001. Precipitating Factors In Pituitary Apoplexy. Journal Of Neurology, Neurosurgery & Psychiatry, 71, 542-545.
- Bret, P.; Jouvet, A.; Madarassy, G.; Guyotat, J. & Trouillas, J. 2001. Visceral Cancer Metastasis To Pituitary Adenoma: Report Of Two Cases. Surgical Neurology, 55, 284-290.
- Carney, J. A.; Gordon, H.; Carpenter, P. C.; Shenoy, B. V. & Go, V. L. W. 1985. The Complex Of Myxomas, Spotty Pigmentation, And Endocrine Overactivity. Medicine, 64, 270-283.
- Chitrasen Yadav, Prof. Pradeep Vaidya, Dr. Laligen Awale, Dr. Geha Raj Dahal, Sanjeeb Jha & Krishna Yadav (2024). Evaluation of Surgical Site Infections and Patterns of Microorganisms involved in Emergency Laparotomy in TUTH . Dinkum Journal of Medical Innovations, 3(08):557-569.
- Chahal, H. S.; Stals, K.; Unterländer, M.; Balding, D. J.; Thomas, M. G.; Kumar, A. V.; Besser, G. M.; Atkinson, A. B.; Morrison, P. J. & Howlett, T. A. 2011. Aip Mutation In Pituitary Adenomas In The 18th Century And Today. New England Journal Of Medicine, 364, 43-50.
- Cheng, R.; Tian, H.; Gao, W. & Li, Z. 2011. A Comparison Between Endoscopic Transsphenoidal Surgery And Traditional Trans-Sphenoidal Microsurgery For Functioning Pituitary Adenomas. Journal Of International Medical Research, 39, 1985-1993.
- El Bakkouri, W.; Hervé, P.; Dzidzinyo, B.; Anis, A.; Louise, B.; Alain, C.; Catherine, V.; Malika, B. & Denis, A. 2016. Visual Disorders Outcome After Endoscopic Endonasal Trans-Sphenoidal Surgery Of Pituitary Macroadenomas. International Journal Of Otolaryngology And Head & Neck Surgery, 5, 134.
- Md. Salah Uddin (2024). Correlation between Duration of Preoperative Motor Deficit and Early Postoperative Motor Functional Recovery in Patients with Intradural Extramedullary Spinal Tumor. Dinkum Journal of Medical Innovations, 3(01):52-63.
- Fassett, D. R. & Couldwell, W. T. 2004. Metastases To The Pituitary Gland. Neurosurgical Focus, 16, 1-4.
- Fernández-Balsells, M. M.; Murad, M. H.; Barwise, A.; Gallegos-Orozco, J. F.; Paul, A.; Lane, M. A.; Lampropulos, J. F.; Natividad, I.; Perestelo-Pérez, L. & Ponce De León-Lovatón, P. G. 2011. Natural History Of Nonfunctioning Pituitary Adenomas And Incidentalomas: A Systematic Review And Metaanalysis. The Journal Of Clinical Endocrinology & Metabolism, 96, 905-912.
- Fernandez, A.; Karavitaki, N. & Wass, J. A. 2010. Prevalence Of Pituitary Adenomas: A Community‐Based, Cross‐Sectional Study In Banbury (Oxfordshire, Uk). Clinical Endocrinology, 72, 377-382.
- Filippa, V. & Mohamed, F. 2006. Acth Cells Of Pituitary Pars Distalis Of Viscacha (< I> Lagostomus Maximus Maximus</I>): Immunohistochemical Study In Relation To Season, Sex, And Growth. General And Comparative Endocrinology, 146, 217-225.
- Gao, Y.; Zheng, H.; Xu, S.; Zheng, Y.; Wang, Y.; Jiang, J. & Zhong, C. 2016. Endoscopic Versus Microscopic Approach In Pituitary Surgery. Journal Of Craniofacial Surgery, 27, E157-E159.
- Gao, Y.; Zhong, C.; Wang, Y.; Xu, S.; Guo, Y.; Dai, C.; Zheng, Y.; Wang, Y.; Luo, Q. & Jiang, J. 2014. Endoscopic Versus Microscopic Transsphenoidal Pituitary Adenoma Surgery: A Meta-Analysis. World Journal Of Surgical Oncology, 12, 1.
- 2018. Bony Anatomy Of Nose Bones Xray Examination The Nasal Bone
- Ironside, J. 2003. Best Practice No 172 Pituitary Gland Pathology. Journal Of Clinical Pathology, 56, 561-568.
- Jagannathan, J.; Yen, C.-P.; Pouratian, N.; Laws, E. R. & Sheehan, J. P. 2009. Stereotactic Radiosurgery For Pituitary Adenomas: A Comprehensive Review Of Indications, Techniques And Long-Term Results Using The Gamma Knife. Journal Of Neuro-Oncology, 92, 345-356.
- Asbin Bandhari, Syeda Hajra Batool, Aatiqa Tariq, Abdullah Hassan, Pooja Bhanarjee & Parshu Ram (2023). A Comprehensive Analysis of Neurosurgeons’ Conversations to Preserve Non-Traditional Brain Networks. Dinkum Journal of Medical Innovations, 2(06):207-216.
- Kelly, D. F.; Barkhoudarian, G.; Griffiths, C. F.; Karimi, K.; Cohan, P. & Ilani, N. 2018. A Patient’s Guide To Endonasal Endoscopic Surgery For Pituitary Adenomas And Related Tumors, California, Saint John’s Health Center.
- Kirk Jr, L. F.; Hash, R. B.; Katner, H. P. & Jones, T. 2000. Cushing’s Disease: Clinical Manifestations And Diagnostic Evaluation. American Family Physician, 62, 1119-27, 1133-4.
- Leestma, J. E.; Walczak, T.; Hughes, J. R.; Kalelkar, M. B. & Teas, S. S. 1989. A Prospective Study On Sudden Unexpected Death In Epilepsy. Annals Of Neurology, 26, 195-203.
- Lenzi, J.; Lapadula, G.; D’amico, T.; Delfinis, C.; Iuorio, R.; Caporlingua, F.; Mecca, N.; Mercuri, V.; Bassotti, G. & Rillo, M. 2015. Evaluation Of Trans-Sphenoidal Surgery In Pituitary Gh-Secreting Micro-And Macroadenomas: A Comparison Between Microsurgical And Endoscopic Approach. Journal Of Neurosurgical Sciences, 59, 11-18.
- Mandeep Karki, Deepak Shrestha, Xiang Zhou, Kailash Kumar Bhandari, Sunima Lama, Rachit Sharma & Rajiv Prasad Shrestha (2024). Simple Decompression versus Anterior Transposition (Submuscular and Subcutaneous) of the Ulnar Nerve in Cubital Tunnel Syndrome: a Meta-Analysis. Dinkum Journal of Medical Innovations, 3(10):700-715.
- Ortiz-Perez, S. & Sánchez-Dalmau, B. 2012. Pituitary Adenomas And Ophthalmology. In: Landolt, A. M. (Ed.) Pituitary Adenomas. Spain: Churchill Livingstone.
- Krishna, G., Chauhan, M., Singh, I., Aggarwal, V., & Kumar, V. (2025). Assessing surgical outcomes in pituitary adenoma: A comparison of microscopic and endoscopic techniques. Surgical Neurology International, 16(234), 1.
- Ram, Z.; Nieman, L. K.; Cutler Jr, G. B.; Chrousos, G. P.; Doppman, J. L. & Oldfield, E. H. 1994. Early Repeat Surgery For Persistent Cushing’s Disease. Journal Of Neurosurgery, 80, 37-45.
- Santos, A. R. L. D.; Fonseca Neto, R. M.; Veiga, J. C. E.; Viana Jr, J.; Scaliassi, N. M.; Lancellotti, C. L. P. & Lazarini, P. R. 2010. Endoscopic Endonasal Transsphenoidal Approach For Pituitary Adenomas: Technical Aspects And Report Of Casuistic. Arquivos De Neuro-Psiquiatria, 68, 608-612.
Publication History
Submitted: February 19, 2025
Accepted: March 02, 2025
Published: April 30, 2025
Identification
D-0419
DOI
https://doi.org/10.71017/djmi.4.4.d-0419
Citation
Bikramaditya Prasad Sah (2025). Outcome Comparison in Microscopic and Endoscopic Trans-Sphenoidal Pituitary Adenoma Surgery in Terms of Extent of Resection. Dinkum Journal of Medical Innovations, 4(04):165-176.
Copyright
© 2025 The Author(s).


