Publication History
Submitted: April 08, 2025
Accepted: April 20, 2025
Published: May 31, 2025
Identification
D-0425
DOI
https://doi.org/10.71017/djmi.4.5.d-0425
Citation
Pushkar Niraula, Madhav Deo & Rajiv Maharjan (2025). Effect of the Short Segment Internal Fixation with Intermediate Inclined Angle Poly Axial Screw at the Fractured Vertebra on the Treatment of Thoracolumbar Fracture at BPKIHS Dharan. Dinkum Journal of Medical Innovations, 4(05):257-272.
Copyright
© 2025 The Author(s).
257-272
Effect of the Short Segment Internal Fixation with Intermediate Inclined Angle Poly Axial Screw at the Fractured Vertebra on the Treatment of Thoracolumbar Fracture at BPKIHS DharanOriginal Article
Pushkar Niraula 1*, Madhav Deo 2, Rajiv Maharjan 3
- B.P. Koirala Institute of Health Sciences, Dharan, Nepal.
- Birat Medical Collage, Biratnagar, Nepal.
- B.P. Koirala Institute of Health Sciences, Dharan, Nepal.
* Correspondence: link2pushkarniraula@gmail.com
Abstract: Fixation at the fracture level along with short segment internal fixation (SSIF) increases the stability and efficacy more than that without the intermediate screw. Short segment internal fixation with straight forward monoaxial screws (SSIF-SFM) are paralleled with the endplate with a relatively short length and it cannot always provide sufficient mechanical support for the anterior column. This hospital-based longitudinal study was conducted for one year at Department of Orthopedics, BPKIHS, Dharan, patients with fracture at thoracolumbar (T1-L5) region without neurological impairment between age of 18 to 80 years who met the inclusion criteria were enrolled. The average duration of the surgery for SSIF-IAP, SSIF-SFM and LSIF were 1.9±0.5/hour, 1.9±0.4/hour and 2.6±0.6/hour respectively. The average length of incision for SSIF-IAP, SSIF-SFM and LSIF were 11.4±1.1cm, 12.3±1.1cm and 16.6±1.1cm respectively. The mean blood loss for SSIF-IAP, SSIF-SFM and LSIF were 214.6±32,7/ml, 245.3±33.9/ml and 301.2±26.9/ml respectively. The average duration of surgery, length of incision and blood loss in the SSIF-IAP group and SSIF-SFM group were significantly decreased compared with those in the LSIF group. The correction loss of AVBH [AVBH (1 week) – AVBH (1 year) / AVBH (1 week)] in the SSIF-SFM group and LSIF group were also decreased compared with those in the SSIF-IAP group at 6-months and the latest follow-up-1year (p < 0.05). The correction loss of the SCA [SCA (1 week) – SCA (1 year) / SCA (1 week)] in the SSIF-IAP group was decreased compared to those in the SSIF-SFM group and LSIF group. There were no significant differences among the three groups concerning correction loss of VBI. Both SSIF-IAP and LSIF can improve the biomechanical stability as compared with SSIF-SFM. However, SSIF-IAP was less extensive compared to LSIF, SSIF-IAP screw system could be an effective alternative way of fixation with satisfactory outcomes minimizing the number of fused levels and promoting rapid relief of back pain and early rehabilitation during the follow-up periods for patients with TL fracture.
Keywords: thoracolumbar fracture, short-segment internal fixation, long-segment internal fixation, inclined-angle screw placement, intermediate screw
- INTRODUCTION
T The thoracolumbar (TL) junction is a transition zone between the rigid thoracic spine and the more mobile lumbar spine (from T11 to L2), and nearly 70 % of all traumatic spinal injuries occur within this region [1,2]. The treatment of TL fracture remains under debate, especially in patients without serious neurological symptoms. Although conservative treatment seems to be effective in the majority of patients, clinical studies have shown that surgical treatment provides better fracture reduction, stronger fixation and long-term clinical outcomes [3, 4]. The posterior approach is often applied for the surgical management of TL fracture [5, 6]. There are two main reasons for this choice. Firstly, more postoperative morbidities are accompanied with the anterior approach as compared with the posterior approach [7-9]. In addition, spine surgeons are more familiar with posterior approach due to its easier application [10]. Short-segment internal fixation (SSIF) via posterior approach is the most common treatment for TL fracture [11]. Although SSIF can obtain satisfactory reduction, it often led to instrumentation failure due to osteoporosis and correction loss [12]. Long-segment internal fixation (LSIF) is an alternative solution, which is stiffer and reduce the load on each screw by the application of longer segmental instrumentation, however, the LSIF is unnecessarily extensive and decrease the flexibility of motion segments. In addition, the LSIF is often associated with the development of adjacent-segment degeneration (ASD) disease [13-15]. Saving the motion segments is the crucial principle of the spinal surgery. Therefore, in order to limit the number of the fusion segments and improve instrumentation efficiency, additional intermediate screws inserted at the fracture level is clinical applied along with SSIF to treat TL fracture [16, 17]. The intermediate screws in this SSIF system were usually paralleled with the superior endplate with relatively short length [18]. However, as a result of collapse of anterior and middle columns in TL fracture, SSIF with straight-forward screws can’t often offer sufficient biomechanical support for the anterior column [19]. Recently, studies [20, 21] have shown that relatively long length pedicle screws could significantly reduce the pull-out force and increase the stiffness of the fixation. We subsequently modified the traditional SSIF with straight-forward screws and developed a new technique for the TL fracture. We changed the direction of implementation of pedicle trajectory as compared with standard implementation, and applied more inclined angle and longer pedicle screws at the fracture level. These intermediate screws traverse all three columns of the vertebral bodies, which can enhance the interface strength and contribute to greater stability with SSIF [22, 23]. The diagnosis, classification and treatment of thoracolumbar spine fractures remain controversial, although conservative treatment is often recommended in the majority of patients. Clinical studies have demonstrated that surgical treatment can lead to better fracture reduction, stronger internal fixation, and more favourable long-term clinical outcomes [24]. Thoracolumbar (TL) junction is a transitional zone between the rigid thoracic spine and the more mobile lumbar spine between the regions of (T11 to L2) and constitutes the majority of all traumatic spinal injuries ranging nearly up to 70% of all cases. The intermediate screws at the fracture level can optimize the load on the instrumentation system and reduce the risk of breaking of screws or rods. Posterior buckling of the rod is more evident within the four-screw fixation construct than within the six-screw fixation construct because the rod of the four-screw fixation construct spans a longer distance between two screws as compared with the six-screw fixation construct. LSIF is unnecessarily extensive, decreases the motion segment and is associated with early adjacent segment degeneration (ASD) [25]. Intermediate screws in the SSIF system are usually paralleled with superior endplates with relatively short lengths. SSIF with a straight-forward monoaxial screw cannot always provide sufficient biomechanical support for the anterior column of the fractured vertebra for unstable thoracolumbar fracture. The intermediate inclined-angle poly axial screw can stabilize the anterior and middle columns of the fractured vertebra and finally improve the stability of the SSIF system. Short Segment Internal Fixation (SSIF) via posterior approach is the most common treatment of thoracolumbar fracture which can obtain a satisfactory reduction but it often leads to the instrumentation failure due to osteoporosis and correction loss [26]. The anterior instrumentation with the bone graft can provide reliable internal fixation, but it is a more invasive approach that is associated with complications and prolonged postoperative recovery [27]. A burst fracture occurs when an axial compressive force on the anterior and middle column collapses the bone and causes failure of the anterior and middle supporting column and typically occurs in a thoracolumbar segment where the lowest thoracic vertebrae connect to the first lumbar vertebrae. The thoracolumbar segment is the most common site for unstable burst fractures, representing approximately 15% of vertebral injuries [28]. Fixation at the fracture level along with short segment internal fixation (SSIF) increases the stability and efficacy more than that without the intermediate screw. Short segment internal fixation with straight forward monoaxial screws (SSIF-SFM) are paralleled with the endplate with a relatively short length and it cannot always provide sufficient mechanical support for the anterior column. Long segment internal fixation (LSIF) system is unnecessarily extensive, decreases the motion segments and is likely to cause adjacent segment degeneration (ASD). The intermediate inclined angle poly axial (IAP) screw can stabilize the posterior and middle columns of the fractured vertebra and improve the stability of the SSIF system. This screw system could be an effective alternative way of fixation with satisfactory outcomes and promote rapid relief of back pain and early rehabilitation during the follow-up periods. Moreover, clinical research has found that the restoration of the fractured vertebral height obtained in SSIF with intermediate angled screws was equivalent to that in LSIF. Only a few literature reviews and studies are available regarding the outcome analysis of the SSIF-IAP screw system, however there are several other factors that determine the outcomes such as osteoporosis (bone density), degree of disc degeneration and variable vertebral size/height etc. However, such types of studies had not been conducted in BPKIHS, Dharan and Eastern/Nepal.
- MATERIALS & METHOD
This is a hospital-based longitudinal study conducted at B.P. Koirala Institute of Health Sciences (BPKIHS), Dharan, Nepal. Patients with TL fracture (T1-L5) without neurological impairment between the ages of 18 to 80 years attended outpatient and ER department of Orthopedics who had given consent and fulfilled inclusion criteria were included in this study. Patients with fracture dislocation, neurological impairment (ASIA A and B), pathological fracture, bilateral pedicle fracture, cauda equina syndrome, previous spine surgery, other major organ system injuries and unable to comply fully with the protocol were excluded from this study. Patients with traumatic TL fracture who has undergone (SSIF-IAP, SSIF-SFM and LSIF) were assessed for the clinical and radiological outcomes during pre and postoperative periods. A detailed clinical history regarding socio-demographic variables like age, gender, mode of injury, site of injury and neurological status in all three (SSIF-IAP, SSIF-SFM, LSIF) screw systems was collected. The preoperative clinical evaluation with VAS/NV-ODI score and relevant investigation including X-ray were done. The preoperative and postoperative VAS/NV-ODI score, VBI, AVBH, and SCA were documented and compared in all three groups at 1 week, 6 months and 1 year. 69 patients who met the criteria for inclusion (44 males and 25 females), ranging from 18 to 78 years old (average of 45±16 years) were enrolled in this study. Patients were divided into three groups: SSIF-IAP: Short segment fixations include poly axial pedicle screw placement one segment above and one segment below the fracture level as well as insertion of screw into the fracture vertebra with an angle of 10° to 20° inclination to the inferior end plate followed by application of rod and cross bridge de connector. Contoured rods using ligamentotaxis to correct the kyphosis and perform the lordotic distraction. SSIF-SFM: Short segment fixations include monoaxial pedicle screw placement one segment above and one segment below the fracture site as well as insertion of screw into the fracture vertebral body followed by application of rod and cross bridge de connector. LSIF: Long Segment fixation includes placement of pedicle screws two segment above and two segment below the fracture level with or without placement of screws into the fractured vertebral body followed by the application of rod and cross bridge de connector.
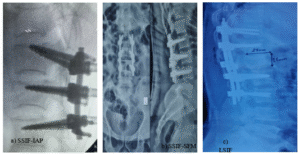
Figure 01. a) SSIF-IAP (short segment internal fixation with inclined angle poly axial) screw. b) SSIF-SFM (short segment internal fixation with straight forward monoaxial) screw. c) LSIF (long segment internal fixation) screw.
Each patient was placed in the prone position on an operating table with arm abduction at 90°and flexion after induction of general anesthesia. Foam padding on chest and over ASIS was kept ensuring the abdominal and chest wall expansion was free. Both shoulders and superior iliac spines were supported by pads to create hyperextension position of the spine and achieve postural reduction. In the SSIF-IAP group, after determination of the fracture level using C-arm, a midline vertical skin incision was made to strip the erector spinae muscles bilaterally, and spinous processes and laminae were then exposed. Standard landmark using intersection method was identified. The starting point was 2 mm superior to the standard landmark, and the insertion of pedicle screws was approximately 10° to 20° inclined to the inferior endplate. Four pedicle screws were bilaterally implanted into adjacent vertebrae above and below the fractured vertebra. Unilateral or bilateral pedicle screws were implanted according to the integrity of the pedicle of the fractured vertebra. The inclined-angle pedicle screws were purchased in the residual lower portion of the injured vertebral body. After all pedicle screws were attached, two rods were applied to connect pedicle screws on both sides using the rod placement system. Minimal distraction was created using the distractor and final tightening of the screws was done at the end. The final reduction and fixation were confirmed by C-arm, and the incision was then irrigated and sutured. Procedure was performed by the different surgeons of department of orthopedic surgery of same institute. The procedure for the SSIF-SFM system, same above steps were followed. Intersection method was applied and pedicle screw placement was done in the fracture vertebrae without creating inclination to the inferior endplate. Whereas in case of LSIF two segment above and two segment below pedicle screw placement was done without placement of screw at the fractured vertebrae. Only instrumentation without bone graft was utilized. The internal fixation stabilization system with poly axial and monoaxial screws about the size of 5.5mm and 6.5mm diameter and 40mm and 45mm length were used in all the procedure depending upon the location of the fracture site and was supplied by Greens, Vishal, Jayon Company of Nepal. All patients were routinely administered prophylactic antibiotics postoperatively for 24 h, and sterile dressing of incision was replaced every 2 days until the suture was removed. Patients were encouraged to start physical activities under the protection of brace. However, excessive and heavy activities were restricted up to 6 weeks after the operation. Following discharge from the hospital, patients were clinically and radiologically assessed at monthly intervals in the orthopedic outpatient clinic up to 1 year. The sample size (n) is calculated according to the formula: n = z² * p * (1 – p) / e². To determine the sample size necessary to estimate with 95% confidence, considering the margin of error as 10%. Z value for a 95% confidence level is 1.96. Assuming a population proportion of 37% following SSIF-IAP had a Mean ODI of 32% (range 14-50) during the 6th-month follow-up postoperative from the study Xiong et al.4 and unlimited population size, the calculated is 80. The ethical approval was obtained from the Institutional Review Committee, BPKIHS (code no. IRC/2388/022). The data were analyzed using Statistical Package for the Social Sciences (SPSS) version 25.0 software for Windows. Numerical data for continuous variables were expressed in the form of mean ± standard deviation. The data for categorical variables were expressed either in number or percentage (n, %), The Kruskal-Walli’s test and Pearson’s Chi-square test were used to observe the association between the categorical variables. The test was considered statistically significant when the p-value <0.05.
- RESULTS & DISCUSSION
In this study, 69 thoracolumbar fractures were included. Demographic data including age, sex, mode of injury, site of injury, and neurological status in the three groups were collected. The mean age of the patient was 46.6±15.8years. Female patients comprised 36% and male 64% of the study participants. The injured vertebral segments were T4 in 1 case, T6 in 1 case, T7 in 2 cases, T10 in 2 cases, T11 in 4 case and T12 in 12 cases, L1 in 30 cases, L2 in 11 cases, L3 in 3 cases and L4 in 3 cases. The fractures were caused by falling from height in 58 cases (82.6%), road traffic accidents in 4 cases (5.8%) and falls on the ground in 8 cases (11.6%). (Table 1). The average length of incision for SSIF-IAP, SSIF-SFM and LSIF were 11.4±1.1cm, 12.3±1.1cm and 16.6±1.1cm respectively. The mean intraoperative blood loss for SSIF-IAP, SSIF-SFM and LSIF were 214.6±32,7/ml, 245.3±33.9/ml and 301.2±26.9/ml respectively. The average duration of the surgery for SSIF-IAP, SSIF-SFM and LSIF were 1.9±0.5/hour, 1.9±0.4/hour and 2.6±0.6/hour respectively (Table 02).
Table 01: Demographic distribution between surgical procedure (n=69)
| Characteristics | Categories | Procedure | p-value | Remarks | ||
| SSIF-IAP | SSIF-SFM | LSIF | ||||
| Gender | Female | 6 (24%) | 7 (28%) | 12 (48%) | 0.217 | Not significant |
| Male | 5 (11.4%) | 9 (20.5%) | 30 (68.2%) | |||
| Mode of Injury | Fall from height | 11 (19.3%) | 14 (24.6%) | 32 (56.1%) | 0.401 | Not significant |
| Road traffic accident | 0 | 1 (25%) | 3 (75%) |
0.359 |
||
| Fall on ground | 0 | 1 (12.5%) | 7 (87.5%) | Not significant | ||
| Site of Injury | Lumbar spine | 9 (19.1%) | 12 (25.5%) | 26 (55.3%) | ||
| Dorsal spine | 2 (9.1%) | 4 (18.2%) | 16 (72.7%) | |||
Table 02: Comparison of Intraoperative parameters (n=69)
| Parameters | SSIF-IAP (n=11) | SSIF-SFM (n=16) | LSIF (n=42) | (p-value) |
| Duration of surgery (hours) | 1.9(1.2-2.5) | 1.9(1.3-2.5) | 2.6(1.5-3.5) | <0.001 |
| Length of incision (cm) | 11.4(10-13) | 12.3(10.5-14.0) | 16.6(14.4-19) | <0.001 |
| Blood loss (ml) | 214(150-290) | 245(210-340) | 301.2(250-370) | <0.001 |
Table 03: Comparison of intraoperative parameters (n=69)
| Parameters | SSIF-IAP & SSIF-SFM (p-value) | SSIF-IAP & LSIF (p-value) | SSIF-SFM & LSIF (p-value) |
| Duration of surgery (hour) | 1.000 | <0.001 | <0.001 |
| Length of incision (cm) | 0.061 | <0.001 | <0.001 |
| Blood loss (ml) | 0.005 | <0.001 | <0.001 |
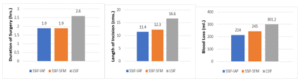
Figure 02: Comparison of surgical parameters in three groups (n=69)
The average VBI for patients who underwent SSIF-IAP was preoperatively 0.6±0.1 and postoperatively during 1 week, 6 months and 1 year were 0.7±0.1, 0.7±0.1, and 0.7±0.1 respectively. The average VBI for patients who undergone SSIF-SFM was preoperatively 0.6±0 and postoperatively during 1 week, 6 months and 1 year were 0.6±0, 0.6±0, and 0.7±0 respectively. The average VBI for patients who underwent LSIF was preoperatively 0.6±0.1 and postoperatively during 1 week, 6 months and 1 year were 0.7±0.1, 0.7±0.1, and 0.7±0.1 respectively. The average AVBH for patients who underwent SSIF-IAP was preoperatively 14.6±0.9/mm and postoperatively during 1 week, 6 months and 1 year were 18.1±0.9/mm, 19.7±1.4/mm, and 19.9±1.4/mm respectively. The average AVBH for patients who underwent SSIF-SFM was preoperatively 15.6±1.5/mm and postoperatively during 1 week, 6 months and 1 year were 17.4±1.5/mm, 17.8±1.8/mm, and 18.2±1.7/mm respectively. The average AVBH for patients who underwent LSIF was preoperatively 15.3±1.4/mm and postoperatively during 1 week, 6 months and 1 year were 16.8±1.6/mm, 17.2±1.6/mm, and 17.2±1.6/mm respectively. The average SCA for patients who underwent SSIF-IAP was preoperatively 15.5±2.4° and postoperatively during 1wk, 6 months and 1 year were 7.0±1.5°, 7.4±1.0°, and 7.2±1.0° respectively. The average SCA for patients who underwent SSIF-SFM was preoperatively 14.1±2.1° and postoperatively during 1 week, 6 months and 1 year were 9.3±1.5°, 8.3±1.2°, and 8.7±1.2° respectively. The average SCA for patients who underwent LSIF was preoperatively 15.4±2.4° and postoperatively during 1 week, 6 months and 1 year were 9.2±2.1°, 8.9±2.0°, and 8.6±1.9° respectively. (Table 04).
Table 04: Comparison of Radiological parameters of surgery in three groups (n=69)
| Radiological parameters | SSIF-IAP | SSIF-SFM | LSIF | p-value | ||||||
| Mean | SD | Median | Mean | SD | Median | Mean | SD | Median | ||
| VBI | ||||||||||
| pre-op | 0.6 | 0.1 | 0.6 | 0.6 | 0.0 | 0.6 | 0.6 | 0.1 | 0.6 | 0.142 |
| 1week | 0.6 | 0.1 | 0.7 | 0.6 | 0.0 | 0.6 | 0.6 | 0.1 | 0.7 | 0.028 |
| 6 months | 0.7 | 0.1 | 0.7 | 0.6 | 0.0 | 0.6 | 0.7 | 0.1 | 0.7 | 0.005 |
| 1year | 0.7 | 0.1 | 0.7 | 0.7 | 0.0 | 0.7 | 0.7 | 0.1 | 0.7 | 0.004 |
| AVBH | ||||||||||
| pre-op | 14.6 | 0.9 | 15.0 | 15.6 | 1.5 | 15.6 | 15.3 | 1.4 | 15.0 | 0.304 |
| 1week | 18.1 | 0.9 | 18.0 | 17.4 | 1.5 | 17.5 | 16.8 | 1.6 | 17.0 | 0.007 |
| 6 months | 19.7 | 1.4 | 19.4 | 17.8 | 1.8 | 17.5 | 17.2 | 1.6 | 17.0 | <0.001 |
| 1year | 19.9 | 1.4 | 20.0 | 18.2 | 1.7 | 18.5 | 17.2 | 1.6 | 17.0 | <0.001 |
| SCA | ||||||||||
| pre-op | 15.5 | 2.4 | 15.0 | 14.1 | 2.1 | 14.0 | 15.4 | 2.4 | 15.5 | 0.114 |
| 1week | 8.2 | 1.5 | 7.0 | 9.3 | 1.5 | 9.0 | 9.9 | 2.1 | 10.0 | 0.048 |
| 6 months | 7.4 | 1.0 | 8.0 | 8.3 | 1.2 | 8.0 | 8.9 | 2.0 | 8.5 | 0.034 |
| 1year | 7.2 | 1.0 | 7.0 | 8.1 | 1.2 | 8.0 | 8.6 | 1.9 | 8.0 | 0.041 |
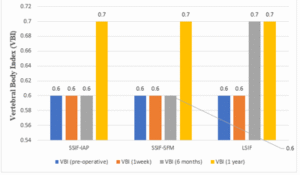
Figure 03: VBI pre and postoperatively at 1 week, 6 months and 1 year in three groups.
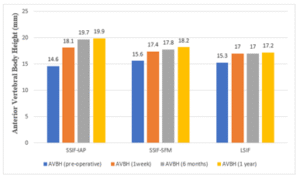
Figure 04: AVBH pre and postoperatively at 1 week, 6 months and 1 year in three groups.
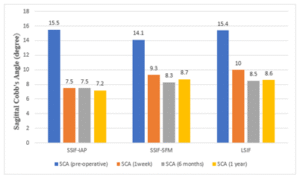
Figure 05: SCA pre and postoperatively at 1 week, 6 months and 1 year in three groups.
The average VAS for patients who underwent SSIF-IAP was preoperatively 8.4±0.7 and postoperatively during 1 week, 6 months and 1 year were 5.5±0.7, 3.8±0.4, and 2.9±0.3 respectively. The average VAS for patients who underwent SSIF-SFM was preoperatively 8.2±0.8 and postoperatively during 1 week, 6 months and 1 year were 5.8±0.8, 4.1±0.5, and 3.3±0.8 respectively. The average VAS for patients who underwent LSIF was preoperatively 8.4±0.7 and postoperatively during 1 week, 6 months and 1 year was 6.0±1.0, 4.5±0.8, and 3.8±0.8 respectively. The average NV-ODI for patients who underwent SSIF-IAP was preoperatively 84±3.7 and postoperatively during 1 week, 6 months and 1 year were 40.4±10.3, 28.3±7.2, and 19.6±3.7 respectively. The average NV-ODI for patients who underwent SSIF-SFM was preoperatively 83.4±4.7 and postoperatively during 1 week, 6 months and 1 year were 46.6±14.4, 32±8.7, and 24.1±5.0 respectively. The average NV-ODI for patients who underwent LSIF was preoperatively 85.5±4.5 and postoperatively during 1 week, 6 months and 1 year were 47.8±11.3, 33.5±6.4, and 27.2±4.2 respectively (Table 05).
Table 05: Comparison of Clinical parameters of surgery in three groups (n=69)
| Clinical parameters | SSIF-IAP | SSIF-SFM | LSIF | p-value | ||||||
| Mean | SD | Median | Mean | SD | Median | Mean | SD | Median | ||
| VAS | ||||||||||
| pre-op | 8.4 | 0.7 | 8.0 | 8.2 | 0.8 | 8.0 | 8.4 | 0.7 | 8.0 | 0.827 |
| 1week | 5.5 | 0.7 | 5.0 | 5.8 | 0.8 | 6.0 | 6.0 | 1.0 | 6.0 | 0.142 |
| 6 months | 3.8 | 0.4 | 4.0 | 4.1 | 0.5 | 4.0 | 4.5 | 0.8 | 4.0 | 0.010 |
| 1year | 2.9 | 0.3 | 3.0 | 3.3 | 0.8 | 3.0 | 3.8 | 0.8 | 4.0 | <0.001 |
| NV-ODI | ||||||||||
| pre-op | 84.0 | 3.7 | 82.0 | 83.4 | 4.7 | 83.0 | 85.5 | 4.5 | 85.5 | 0.238 |
| 1week | 40.4 | 10.3 | 38.0 | 46.6 | 14.4 | 40.0 | 47.8 | 11.3 | 44.0 | 0.058 |
| 6 months | 28.3 | 7.2 | 26.0 | 32.0 | 8.7 | 29.0 | 33.5 | 6.4 | 32.0 | 0.024 |
| 1year | 19.6 | 3.7 | 18.0 | 24.1 | 5.0 | 22.0 | 27.2 | 4.2 | 28.0 | <0.001 |
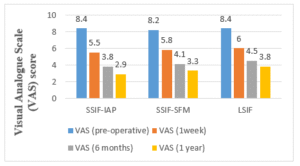
Figure 06: VAS pre and postoperatively at 1 week, 6 months and 1 year in three groups.
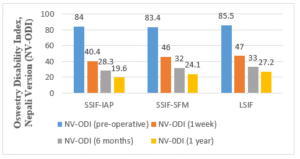
Figure 07: NV-ODI pre and postoperatively at 1 week, 6 months and 1 year in three groups.
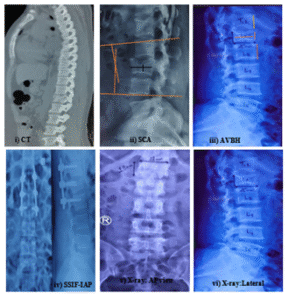
Figure 08: i) CT showing L1 Burst fracture. ii) L3 Burst fracture, SCA (Sagittal Cobb’s angle) calculation. iii) AVBH (anterior vertebral body height) calculation. iv) SSIF-IAP (short segment internal fixation with inclined angle poly axial) screw. v) X-ray: LS spine anteroposterior view. vi)X-ray: LS spine lateral view.
Table 06: Comparison of parameters (Correction Loss) of surgery in three groups (n=70)
| Correction Loss | VBI | VBI (%) | AVBH | AVBH (%) | SCA | SCA (°) |
| SSIF-IAP | 0.166 | 16.66% | 0.099 | 9.94% | 0.028 | 2.85° |
| SSIF-SFM | 0.164 | 16.14% | 0.045 | 4.5% | 0.052 | 5.23° |
| LSIF | 0.166 | 16.62% | 0.023 | 2.38% | 0.065 | 6.5° |
The correction loss of VBI (%) in SSIF-IAP, SSIF-SFM, and LSIF were 0.166 (16.66%), 0.164 (16.14%), and 0.166 (16.62%) respectively. The correction loss of AVBH (%) in SSIF-IAP, SSIF-SFM, and LSIF were 0.099 (9.94%), 0.045 (4.5%), and 0.023 (2.38%) respectively. The correction loss of SCA in SSIF-IAP, SSIF-SFM, and LSIF were 0.028 (2.85°), 0.052 (5.23°), and 0.065 (6.5°) respectively (Table 06).
Table 07: Comparison of Clinical and Radiological parameters of surgery in three groups (n=70)
| SSIF-IAP & SSIF-SFM | SSIF-IAP & LSIF | SSIF-SFM & LSIF | |
| VAS | (p-value) | (p-value) | (p-value) |
| pre-op | 0.631 | 0.933 | 0.564 |
| 1week | 0.301 | 0.067 | 0.304 |
| 6 months | 0.103 | 0.007 | 0.086 |
| 1 year | 0.177 | <0.001 | 0.018 |
| NV-ODI | |||
| pre-op | 0.636 | 0.298 | 0.127 |
| 1week | 0.111 | 0.023 | 0.360 |
| 6 months | 0.161 | 0.010 | 0.177 |
| 1 year | 0.012 | <0.001 | 0.020 |
| VBI | |||
| pro-op | 0.410 | 0.551 | 0.045 |
| 1week | 0.004 | 0.183 | 0.079 |
| 6 months | 0.001 | 0.023 | 0.123 |
| 1year | <0.001 | 0.007 | 0.441 |
| AVBH | |||
| pro-op | 0.140 | 0.228 | 0.492 |
| 1week | 0.116 | 0.003 | 0.131 |
| 6 months | 0.009 | <0.001 | 0.199 |
| 1year | 0.013 | <0.001 | 0.033 |
| SCA | |||
| pre-op | 0.116 | 0.868 | 0.047 |
| 1week | 0.113 | 0.017 | 0.367 |
| 6 months | 0.061 | 0.013 | 0.397 |
| 1year | 0.064 | 0.014 | 0.509 |
DISCUSSION
Both conservative and surgical management can be used in the treatment of TL fractures. Conservative management is often accompanied by discomfort and limited mobility. Surgical management in patients with thoracolumbar junction fracture can maintain reduction, improve early mobilization and prevent further deformity and neurologic deterioration. An author [26] reported there was screw breakage in the SSIF-SFM screw system and screw loss in the LSIF with an instrumentation failure rate of 2.90% and instrumentation failure rate with screw breakage at 6-month follow-up was 4.16%. Short-segment fixation for thoracolumbar junction fractures results in kyphosis correction and the maintenance of the sagittal alignment similar to a long-segment fixation. Both SSIF-IAP and LSIF can improve the biomechanical stability as compared with SSIF-SFM. Moreover, SSIF-IAP was an effective and reliable operative technique for patients with Denis’s type B thoracolumbar fracture [26]. An author [27] demonstrated there were no significant radiological and functional differences between intermediate segment and long segment fixation in thoracolumbar burst fracture. An author [30] determined the efficacy of short segment with index vertebra fixation for thoracolumbar fractures and reported duration of hospitalization, the operative times and perioperative blood loss were significantly reduced in patients undergoing short segment fixation. An showed there was no clinical outcomes difference between the short-segment and long-segment fixation but radiographic indexes were better in the long-segment fixation group with a decreased rate of implant failure. An author [32] reported the short-segment pedicle screws fixation was not significantly different from the long-segment pedicle screws fixation in terms of improvement of back pain and return to work and also in correction of kyphotic deformity. An author [33] reported reduction of unstable thoracolumbar injuries even with≥7 score on load sharing classification and maintenance with short segment fixation including the fractured vertebra and avoid the need for anterior reconstruction. SSIF with intermediate screws theoretically corrects kyphotic deformity but not able to provide adequate support to the anterior column of the fractured vertebra for unstable thoracolumbar fracture. Modification in SSIF with inclined angle intermediate poly axial screws can increase the length of pedicle screws, increase the pull-out strength and provide greater construct stiffness. The pedicle screws in the SSIF-IAP group were inserted into the lower residual portion of the injured vertebral body, which would contribute to the pull-out strength [34]. He [35] explained the “Eggshell” effect was created when the vertebral height was fully restored by the internal fixation device but the compressed bone trabeculae were not restored in the injured vertebral body. An author [36] reported intermediate screws in the SSIF-SFM were paralleled with the superior endplate, and the end portion of screws in the eggshell-like cavity cannot provide additional interface strength. Nevertheless, an inclined angled screw can escape from this cavity and contribute to greater strength. It minimizes negative effects caused by the “eggshell” deformity and promotes fracture healing by increasing structural stability. However, no data are available to support this assumption which needs to be verified by further biomechanical study. An author [37] studied the clinical and biomechanical effects of adding an intermediate screw to the fractured vertebra and concluded that this technique increases construct stiffness and shields the fractured vertebral body from anterior loads. An author [38] indicated that the addition of posterior fixation points could significantly increase the stiffness of pedicle screw fixation for burst fractures and more fixation points could theoretically reduce the stress on the individual instrument components. An author [39] reported 39% screw breakage and 23% reoperation rate in a case series of thoracolumbar fracture treated with variable screw placement or isolated instrumentation and arthrodesis. An author [40] showed that there was highest failure rate about 50% of the hardware with cotrel- Dubousset instrumentation used in short segment fixation with thoracolumbar fracture. An author [41] reported transpedicular fixation two levels above the kyphosis should be used at the thoracolumbar junction where compressive forces act more anteriorly. Fixation two levels above the fracture site were to prevent the progression of kyphosis as well as hardware failure. Whereas, fixation one level distal to the fracture site was to preserve the motion segment. Traditional SSIF with intermediate screws theoretically corrects kyphotic deformity. This instrumentation system is not able to provide adequate support to the anterior column of the fractured vertebra for unstable thoracolumbar fractures. The modification of SSIF with inclined angle intermediate screw has the advantage to increase the length of screw which then by increases the pullout strength and provide the strong construct. As the short segment fixation has its own benefits in compromising the duration of surgery and unnecessary length of incision at the surgical site which play vital role in decrease in amount of blood loss intraoperatively as well as early wound recovery and mobilization. The confounders of study are osteoporosis and age. The bone density, degree of disc degeneration and vertebral height/size are variable. The clinical observation was based on data from relatively healthy strong bones and different picture might emerge in osteoporotic bones. The study is for short term and on small population done by different surgeon using different surgical technique and different hardware system at the same center. Thus, the clinical outcomes and the finding may be biased. Limited literature reviews and articles are available and the speculation of this study was based on clinical observations. Long term biomechanical outcomes research needed to support this study. In our study of 69 patients with thoracolumbar fractures who were treated with three different internal fixation systems, no significant demographic variations were observed among the three groups (Table 01). The average values of length of incision, duration of surgery and blood loss in the SSIF-IAP group and SSIF-SFM group were significantly decreased compared with those in the LSIF group (p<0.001) (Table 02). There were no significant differences between the SSIF-IAP group and the SSIF-SFM group concerning length of incision (p≈0.061) and length of surgery (p≈1.00) whereas significant decrease in blood loss was found (p<0.005). (Figure 1). There were significant differences and improved among the three groups concerning the VAS score at the pre-operation and 6-months (p≈0.010) and last follow-up at 1 year (p<0.001). (Table 5). The VAS scores in the SSIF-IAP group and SSIF-SFM group were decreased compared with those in the LSIF group at the 6-months (p≈0.007) and the latest follow-up at 1 year (p<0.001) whereas no significant difference was observed between the group of SSIF-IAP and SSIF-SFM at 6 months (p≈0.103) and last follow-up at 1 year (p≈0.177). The NV-ODI score following the operation was also significantly improved in all three groups (p<0.05) with a significant difference in the last follow-up score at 1 year (p<0.001). (Table 5). Similarly, there were significant differences among SSIF-IAP groups and LSIF groups at 6 months (p≈0.010) and last follow-up at 1 year (p<0.001) but no obvious differences were observed between SSIF-IAP and SSIF-SFM group at 6 months (p≈0.161) and last follow-up at 1 year (p≈0.012). (Table 07). Overall improvements in VBI, AVBH and SCA of the fractured vertebra following the operation were observed among the three groups (p<0.05). (Table 04). There was significant difference in VBI between the SSIF-IAP and LSIF at postoperative period of 6 months (p≈0.023) and last follow-up at 1 year (p≈0.007). VBI in between the SSIF-IAP group and SSIF-SFM group were also significantly improved at 6 months (p≈0.001) and the latest follow-up at 1 year (p<0.001). (Table 7). AVBH in between the SSIF-IAP group and LSIF group were improved during postoperative period of follow-up at 6 months (p<0.001) and 1 year (p<0.001). Similarly, there were significant difference in value comparing between the SSIF-IAP groups and SSIF-SFM groups at 6 months (p≈0.009) and last follow-up at 1 year (p≈0.013). (Table 07). There were no significant differences in SCA between the SSIF-IAP group and the SSIF-SFM group postoperatively at 6 months (p≈0.061) and last follow-up at 1 year (p≈0.064). SCA in between the SSIF-IAP group and LSIF group were significantly improved at 6-months (p≈0.013) and last follow-up at 1 year (P<0.014). Similarly, there were no significant differences among the three groups concerning the correction losses of VBI (P>0.05). However, the correction losses of AVBH in the SSIF-SFM group and LSIF group were decreased compared with those in the SSIF-IAP group. The correction losses of SCA in the SSIF-IAP group decreased compared with those in the SSIF-SFM and LSIF group (Table 6). Values of all considered parameters (length of incision, duration of surgery, blood loss) in the LSIF group were the highest among the three groups. No significant differences were observed between the SSIF-IAP group and SSIF-SFM group regarding these parameters. Improvements of functional outcomes (VAS back pain and NV-ODI) were obtained in the SSIF-IAP group and SSIF-SFM group as compared with those in the LSIF group at the 6-month and the last follow-up at 1 year. Favourable surgical outcomes can be defined by 15% improvement in ODI score [42], and our data were consistent with this criterion. These results suggested that intermediate inclined-angle screw insertion at the fracture level did not significantly increase the surgical duration and the blood loss as compared with the traditional straight-forward screw insertion. Although there was no significant difference among the three groups with regard to VBI. However, changes of AVBH and SCA were observed postoperatively. The initial correction of AVBH and SCA in the SSIF-IAP group was better than SSIF-SFM group and LSIF group.
- CONCLUSION
In conclusion, this study demonstrates that the SSIF-IAP technique offers significant advantages over conventional LSIF and SSIF-SFM approaches in the surgical management of thoracolumbar fractures without neurological impairment. Compared with LSIF, SSIF-IAP achieved shorter operative duration, smaller incision length, and reduced intraoperative blood loss, while maintaining comparable biomechanical stability. Although SSIF-SFM showed favorable results in reducing correction loss of AVBH, SSIF-IAP provided superior maintenance of SCA and preserved vertebral height with greater pull-out strength. Importantly, SSIF-IAP minimized the number of fused levels, facilitating earlier postoperative recovery and rehabilitation. Collectively, these findings suggest that the intermediate inclined angle polyaxial screw system represents an effective and less invasive alternative to LSIF, with satisfactory clinical and radiological outcomes for patients with thoracolumbar fractures during follow-up.
REFERENCES
- P Leucht KF, G Muhr, EJ Mueller: Epidemiology of traumatic spine fractures. Injury 2009, 40(2):166-172.
- Tian Y ZY, Yin B, Zhang F, Liu B, Chen W, Zhang Y: Age- and gender-specific clinical characteristics of acute adult spine fractures in China. Int Orthop 2016, 40(2):347–353.
- Siebenga J LV, Segers MJ, Elzinga MJ, Bakker FC, Haarman HJ, Rommens PM, ten Duis HJ, Patka P: Treatment of traumatic thoracolumbar spine fractures: a multicenter prospective randomized study of operative versus nonsurgical treatment. Spine (Phila Pa 1976) 2006, 31(25):2881-2890.
- Prabin Kumar Jha, Dr. Bindu Laxmi Shah, Dr. Shruti Kumari Thakur & Dr. Avinash Thakur (2024). Effectiveness of Dexamethasone as an Adjuvant to Bupivacaine in Supraclavicular Brachial Plexus Block. Dinkum Journal of Medical Innovations, 3(01):13-25.
- W D: Innere Fixation von Brust- und Lendenwirbelfrakturen. Aktuel Probl Chir Orthop 1984, 28:1-125.
- Roy-Camille R SG, Maze1 C: Internal fixation of the lumbar spine with pedicle screw plating. Clin Orthop 1986, 203:7-17.
- Shono Y MP, Cunningham BW: Experimental study of thoracolumbar burst fractures. A radiographic and biomechanical analysis of anterior and posterior instrumentation systems. Spine (Phila Pa 1976) 1994, 19(15):1711-1722.
- Sasso RC RK, Hanson D, Reilly T, McGuire RA Jr, Best NM: Unstable thoracolumbar burst fractures: anterior-only versus short-segment posterior fixation. J Spinal Disord Tech 2006, 19(4):242-248.
- Sasso RC BN, Reilly TM, McGuire RA Jr: Anterior-only stabilization of three-column thoracolumbar injuries. J Spinal Disord Tech 2005, 18 Suppl:S7-14.
- Nahal Mostak Khan, Soheb Ahmed Robin, Lutfullahil Khabir & Sohel Mahmud (2024). Role of Vitamin C in Development of Age Related Cataract. Dinkum Journal of Medical Innovations, 3(01):26-34.
- Mahar A KC, Wedemeyer M, Mitsunaga L, Odell T, Johnson B, Garfin S: Short-segment fixation of lumbar burst fractures using pedicle fixation at the level of the fracture. Spine (Phila Pa 1976) 2007, 32(14):1503-1507.
- McLain RF SE, Benson DR: Early failure of short-segment pedicle instrumentation for thoracolumbar fractures. A preliminary report. J Bone Joint Surg Am 1993, 75(2):162-167.
- Nagata H SM, Transfeldt EE, Lewis JL: The effects of immobilization of long segments of the spine on the adjacent and distal facet force and lumbosacral motion. Spine (Phila Pa 1976) 1993, 18(16):2471-2479.
- Dekutoski MB SM, Ogilvie JW, Olsewski JM, Wallace LJ, Lewis JL: Comparison of in vivo and in vitro adjacent segment motion after lumbar fusion. Spine (Phila Pa 1976) 1994, 19(15):1745-1751.
- Md. Salah Uddin (2024). Correlation between Duration of Preoperative Motor Deficit and Early Postoperative Motor Functional Recovery in Patients with Intradural Extramedullary Spinal Tumor. Dinkum Journal of Medical Innovations, 3(01):52-63.
- Wang H ZY, Li C, Liu J, Xiang L: Comparison of Open Versus Percutaneous Pedicle Screw Fixation Using the Sextant System in the Treatment of Traumatic Thoracolumbar Fractures. Clin Spine Surg 2017, 30(3):E239-E246.
- Li K LZ, Ren X, Xu H, Zhang W, Luo D, Ma J: Effect of the percutaneous pedicle screw fixation at the fractured vertebra on the treatment of thoracolumbar fractures. Int Orthop 2016, 40(6):1103-1110.
- Guven O KB, Bezer M, Aydin N, Nalbantoglu U: The use of screw at the fracture level in the treatment of thoracolumbar burst fractures. J Spinal Disord Tech 2009, 22(6):417-421.
- Tezeren G KI: Posterior fixation of thoracolumbar burst fracture: short-segment pedicle fixation versus long-segment instrumentation. J Spinal Disord Tech 2005, 18(6):485-488.
- Kayanja M EK, Milks R, Lieberman IH: The mechanics of polymethylmethacrylate augmentation. Clin Orthop Relat Res 2006, 443(124-30).
- Yang SC LP, Tu YK: Pullout evaluation of sawbone experiment in different types of pedicle screws combined with bone cement augmentation for severe osteoporotic spine. Acta Bioeng Biomech 2018, 20(2):55-64.
- Feng ZZ CY, Jiang C, Jiang XX: Short-term outcome of bilateral decompression via a unilateral paramedian approach for transforaminal lumbar interbody fusion with unilateral pedicle screw fixation. Orthopedics 2011, 34(5):364.
- Xiao YX CQ, Li FC: Unilateral transforaminal lumbar interbody fusion: a review of the technique, indications and graft materials. J Int Med Res 2009, 37(3):908-917.
- Boisclair D M-TJ, Parent S, Petit Y: Compressive loading of the spine may affect the spinal canal encroachment of burst fractures. J Spinal Disord Tech 2013, 26(6):342-346.
- Acharya RS, AI-Oraibi S, Adhikari S P et al. Validation in the Cross-cultural adaptation of the Nepali version of the Oswestry disability index. Indian Journal of Physiotherapy and Occupational Therapy. 2014; 8(2):158-63.
- Xiong C, Huang B, Wei T et al. Effect of the short segment internal fixation with intermediate inclined angle polyaxial screw on the treatment of Denis type B thoracolumbar fracture. Journal of Orthopaedic Surgery and Research. 2020; 15(1):1-1.
- Dipesh Pariyar, Rishi Bista & Rajaram Maharjan (2024). Ankle Brace V/s below Knee Slab in Lateral Ankle Sprains (Grade I and II). Dinkum Journal of Medical Innovations, 3(11):750-760.
- Kose KC, Inanmaz ME, Isik C et al. Short segment pedicle screw instrumentation with an index level screw and cantilevered hyperlordic reduction in the treatment of type-A thoracolumbar spine. The bone & joint journal. 2014; 96(4):541-7.
- Butt MF, Farooq M, Mir B et al. Management of unstable thoracolumbar spinal injuries by posterior short segment spinal fixation. International Orthopaedics. 2007; 31:259-64.
- Agrawal H, Sharma A, Singh V et al. Long segment fixation versus short segment fixation with instrumentation of index vertebra for thoracolumbar burst fractures. Surgical Neurology International. 2022; 13:233.
- Li J, Liu L. Comparison of short segment versus long segment fixation for the treatment of thoracolumbar burst fracture: a meta-analysis. Int J Clin Exp Med. 2017; 10(10):1750-62.
- Aly TA. Short segment versus long segment pedicle screws fixation in management of thoracolumbar burst fractures: Meta-Analysis. Asian Spine Journal. 2017; 11(1):150-60.
- Kanna RM, Shetty AP, Rajasekaran S et al. Posterior fixation including the fractured vertebra for severe unstable thoracolumbar fractures. The Spine Journal. 2015; 15(2):256-64.
- Ruiz FK, Bohl DD, Webb ML et al. Oswestry Disability Index is a better indicator of lumbar motion than the Visual Analogue Scale. The Spine Journal. 2014; 14(9):1860-5.
- He D, Wu L, Sheng X et al. Internal fixation with percutaneous kyphoplasty compared with simple percutaneous kyphoplasty for thoracolumbar burst fractures in elderly patients: a prospective randomized controlled trial. European Spine Journal. 2013; 22:2256-63.
- Xu BS, Tang TS, Yang HL. Long-term results of thoracolumbar and lumbar burst fractures after short-segment pedicle instrumentation, with special reference to implant failure and correction loss. Orthopaedic Surgery. 2009; 1(2):85-93.
- Mahar A, Kim C, Wedemeyer M, et al. Short-segment fixation of lumbar burst fractures using pedicle fixation at the level of the fracture. Spine. 2007; 32(14):1503-7.
- Anekstein Y, Brosh T, Mirovsky Y et al. Intermediate screws in short segment pedicular fixation for thoracic and lumbar fractures: a biomechanical study. Clinical Spine Surgery. 2007; 20(1):72-7.
- Alvine GF, Swain JM, Asher MA et al. Treatment of thoracolumbar burst fractures with variable screw placement or Isola instrumentation and arthrodesis: case series and literature review. Clinical Spine Surgery. 2004; 17(4):251–64.
- McLain RF, Sparling E, Benson DR et al. Early failure of short-segment pedicle instrumentation of thoracolumbar fractures. A preliminary report. JBJS. 1993; 75(2):162-7.
- Carl AL, Tromanhauser SG, Roger DJ et al. Pedicle screw instrumentation for thoracolumbar burst fractures and fractures dislocations. Spine. 1992; 17:317-24.
- Casal-Moro R, Castro-Menendez M, Hernandez-Blanco M, et al. Long-term outcome after microendoscopic disectomy for lumbar disc herniation: a prospective clinical study with a 5-year follow-up. Neurosurgery. 2011; 68(6):1268-75.
Publication History
Submitted: April 08, 2025
Accepted: April 20, 2025
Published: May 31, 2025
Identification
D-0425
DOI
https://doi.org/10.71017/djmi.4.5.d-0425
Citation
Pushkar Niraula, Madhav Deo & Rajiv Maharjan (2025). Effect of the Short Segment Internal Fixation with Intermediate Inclined Angle Poly Axial Screw at the Fractured Vertebra on the Treatment of Thoracolumbar Fracture at BPKIHS Dharan. Dinkum Journal of Medical Innovations, 4(05):257-272.
Copyright
© 2025 The Author(s).


