Publication History
Submitted: July 08, 2025
Accepted: July 28, 2025
Published: July 31, 2025
Identification
D-0450
DOI
https://doi.org/10.71017/djmi.4.7.d-0450
Citation
Krishna Bahadur Bista, Bhupendra Man Singh Shrestha & Bodh Raj Gautam (2025). To Find Out the Correlation between Clinical Features and MRI Findings in Cases of Lumbar Disc Prolapse. Dinkum Journal of Medical Innovations, 4(07):426-439.
Copyright
© 2025 The Author(s).
426-439
To Find Out the Correlation between Clinical Features and MRI Findings in Cases of Lumbar Disc ProlapseOriginal Article
Krishna Bahadur Bista 1, Bhupendra Man Singh Shrestha * 2, Bodh Raj Gautam 3
- Associate Professor, Dept. of Orthopedics & Trauma Surgery, Gandaki Medical College Teaching Hospital and Research Center, Pokhara, Nepal.
- Dept. of Orthopedics & Trauma Surgery, Gandaki Medical College Teaching Hospital and Research Center, Pokhara, Nepal.
- Dept. of Orthopedics & Trauma Surgery, Gandaki Medical College Teaching Hospital and Research Center, Pokhara, Nepal.
* Correspondence: sthabhupendra1305@gmail.com
Abstract: Lower back pain has emerged as a major public health problem, and one of the most prominent causes is lumbar disc herniation (LDH). The successful management of LDH requires thorough clinician evaluation and proper correlation with MRI findings. This study was conducted to observe the correlation between clinical and MRI findings in patients with Lumbar disc prolapse and performed in the Department of Orthopedics and Trauma Surgery, Gandaki Medical College & Teaching Hospital, Tribhuvan University, Pokhara, for one and a half years. One hundred fourteen clinically diagnosed patients of LDH within the age group 18-50 years were evaluated clinically on pain distribution, neurological signs, and symptoms; and radiologically assessed with an MRI of lumbosacral spine. The MRI evaluation included types and levels of disc herniation, neural foramen compromise, and nerve root compression. These MRI findings were correlated with clinical findings. Statistical analysis (Pearson’s Correlation and Kappa Coefficient) was done using the latest version of SPSS. Kappa coefficient value ≥0.5 was used as a good agreement at a 95% level of significance i.e. p-value < 0.05 was considered statistically significant. Out of 114 patients, 56 (49.12%) were males and 58 (60.88%) were females. The mean age was 53.98 ± 13.065 years (range 21-79 years). There was no statistically significant correlation between types of disc herniation, neural foramen compromise, and MRI level S1 with Neurological deficit; Radicular pain and neurological deficit; and clinical level S1 respectively (p-value>0.05). There was a significant correlation of Radicular Pain, SLRT, and Neurological deficit (motor and sensory) with the Nerve root compression in MRI of lumbar spine levels at the L5 level with no significant correlation at the S1 Level. There was no correlation between MRI findings of disc herniation, neural foramen compromise, and Clinical parameters of radicular pain, or neurological deficit.
Keywords: clinical correlation, magnetic resonance imaging, lumbar disc herniation
- INTRODUCTION
Lumbar disc herniation (LDH) is the displacement of the contents of the intervertebral disc (nucleus pulposus) through the external membrane (annulus fibrosus) generally at the posterolateral region [1]. LDH may cause compression and irritation of lumbar nerve roots and the dural sac, clinically represented as sciatica. The lifetime prevalence of having LBP is as high as 80% with the global burden of LDH ranging from 6.3% to 10.4 %.70 The primary signs and symptoms of lumbar disc herniation include radicular pain, and sensory abnormalities, accompanied as well with motor weakness in the distribution of one or more lumbosacral nerve roots. The affected dermatome varies based on the level of herniation as well as the herniation type [2]. The recent advent of magnetic resonance imaging (MRI) has provided clinicians with a noninvasive mechanism for viewing lumbar anatomy in great detail with a diagnostic accuracy of as high as 97%, but with high inter-observer reliability [3]. The findings of disc pathology in MRI do not correlate with the likelihood of chronic pain including other symptoms or the need for surgery in the future. Milette et al. found that loss of disc height or abnormal signal intensity is highly predictive of symptomatic tears and the presence of a disc bulge or protrusion does not have additional significance. Borenstein and others clearly opined that MRI findings were not predictive of the development or duration of low back pain and that clinical correlation is essential. An author [4] found that the presence of disc extrusion and severe nerve root compression at one or multiple sites is strongly associated with distal leg pain. In a recent meta-analysis of 20 studies evaluating the MRI of asymptomatic people, they reported disc abnormalities at any level were reduction in signal intensity (20–83%), disc bulges (10–81%), disc protrusion (3–63%), disc extrusion (0–24%), disc narrowing (3–56%), and AF tears (6–56%). A herniated disc on imaging studies must be correlated with objective clinical findings, otherwise, it may be presumed to be an asymptomatic herniation [5] There is a paucity of literature regarding the importance of MRI in patients with lumbar disc prolapse and MRI findings which are clinically significant and aid in the management of the condition. Hence in keeping in mind the gap in the available literature, the present study was conducted to determine the association between patients’ clinical features including pain distribution, neurological signs, and symptoms in lumbar disc prolapse and MRI findings. An author [6] correlated the abnormalities observed on MRI and clinical features of lumbar disc prolapse of 119 clinically diagnosed patients with lumbar disc prolapse were included in the study. Clinical evaluation included pain distribution, neurological symptoms, and signs. MRI evaluation included grades of disc degeneration, type of herniation, neural foramen compromise, nerve root compression, and miscellaneous findings. They observed that the presence of Centro-lateral protrusion or extrusion with gross foramen compromise correlates with clinical signs and symptoms very well, while central bulges and disc protrusions correlate poorly with clinical signs and symptoms. The presence of neural foramen compromise is more important in determining the clinical signs and symptoms while the type of disc herniation (bulge, protrusion, or extrusion) correlates poorly with clinical signs and symptoms. An author [7] observed the correlation between the abnormalities observed on magnetic resonance imaging (MRI) and clinical features in patients of lumbar disc prolapse. The authors observed dermatological pain, neurological symptoms, and deficit in 123, 73, and 36 patients respectively. On MRI; disc bulges, protrusion, and extrusion were seen in 208, 56, and 26 levels, respectively. Among 66 patients with root compression, 57 were symptomatic with radicular pain while 23 had neurological deficits. 20 cases each were asymptomatic in cases of 31 central disc protrusion and 23 Centro-lateral protrusion, whereas, 2 cases were asymptomatic in groups with far lateral disc protrusion. Out of 10 cases having central disc extrusion, only five were symptomatic and all 16 Centro-lateral cases of disc extrusions were symptomatic. MRI evidence of neural root or foramen compromise with a disc bulge, protrusion, or extrusion with symptoms had an odd ratio of 41.7 and 6.0 respectively. Patients with even gross extrusion and central protrusion but not compromising neural foramen were asymptomatic. Thus, there was no statistical correlation between clinical symptoms and MRI findings like disc bulge, disc protrusion, and disc extrusion. Lumbar disc prolapse is one of the most common causes of low back pain, usually seen in the working population, and has led to significant morbidity [8]. However, there are contradictory reports regarding the significance of MRI findings seen in these patients regarding if MRI is essential in every case of lumbar disc prolapse and if MRI is performed, which of the findings would be clinically significant and which of those findings would be important for the management of the patient. Proper correlation of the clinical evaluations and radiological findings is needed to avoid unnecessary surgical interventions in patients with radiological findings alone [9]. So, our study was conducted to correlate the clinical features of lumbar disc prolapse with abnormalities observed on MRI, thus to know about the significance while managing those cases. This study correlated between clinical and MRI findings of lumbar disc prolapse with radiculopathy and assessed the clinical features of the patients with lumber disc prolapse with radiculopathy.
- MATERIALS & METHOD
This is a hospital-based cross-sectional observational study. The study is carried out in the Department of Orthopedics and Trauma Surgery, GMCTH (Emergency, Inpatient & Outpatient) for a period of one year. Study Population included 114 patients presenting in the Orthopedics OPD and Emergency of GMCTH. Non-probability sampling technique is used and Sample size in estimating the population proportion n is (Cochrane’s Formula).
𝑛 = 𝑍2 (1 − 𝑝)/𝑒2
Where:
𝑍𝛼/2=the critical value of Z for a (1- a) × 100%
Confidence that cuts off a right-tail area of ½a under the standard normal curve, e.g. Z = 1.96 for a 95% confidence.
p = Estimate of true population proportion = 0.08
e = margin of error = 0.05
Sample Size: 114
All patients fulfilling the inclusion criteria were requested for informed consent. The presence of deformity, duration of symptoms, the side of the pain, and dermatomal level of pain distribution were recorded. The clinical examination included the straight leg raising test, and neurological examination of B/L lower limb (motor, sensory, knee, and ankle jerk). Muscle power grading was done by the Medical Research Council (MRC) and sensory grading was done as per ASIA (American Spinal Cord Injury Association). Neurological deficient taken as motor, power ≤3/5, and sensory ≤1/2. The MRI evaluation included type, level, and position of disc herniation, level of neural foramen compromise, and nerve root compression. These MRI findings were then correlated with clinical signs and symptoms. Statistical analysis (Pearson’s Correlation and Kappa Coefficient) was done using the latest version of SPSS software. A kappa coefficient value of 0.5 and above was used as a good agreement at a 95% level of significance i.e. p-value < 0.05 was considered statistically significant. This is a “self-structured proforma”, designed and adopted by the experts at the Department of Orthopedics and Trauma Surgery, GMCTH, Pokhara. It was used for the collection of the information required for the purpose of this study. The study started after approval from the Institutional Review Board. Eligible patients were requested for informed written consent before enrolling in the study. All patients who provided informed consent were enrolled. No extra financial burden was given to the patients.
Table 01: Criteria for dermatological level
| Root Involvement | Pain Location | Muscle weakness | Sensory Distribution | Reflex change:
Diminished/Absent |
| L3 | Anterior thigh, knee | Hip flexion, hip adduction, knee extension | Lower medial thigh | Knee Jerk |
| L4 | Lower anterior knee, medial aspect of leg and ankle | Knee extension, ankle dorsiflexion | The medial part of the lower leg | Knee jerk |
| L5 | The anterolateral aspect of the leg and dorsum of the foot | Ankle dorsiflexion, great toe extension, ankle eversion, hip abduction and internal rotation | Anterior lateral lower, leg, dorsum of the foot, and great toe. | None |
| S1 | Posterolateral leg extending into lateral toes and heel | Ankle plantar flexion and toe flexion | Lateral foot, 4th and 5th toe, and sole of foot. | Ankle jerk |
The criteria used to determine the dermatomal level were [10]. Non-Specific: Pain in the gluteal region or posterior aspect of the thigh or any other patterns that do not fit into any of the above categories. When the leg pain distribution involves more than one dermatomal level, it was recorded as symptomatic of two levels or more depending on the areas involved. Neural canal compromise was graded as thecal sac compression, neural foramen or lateral recess compromise, and nerve root impingement. Neural foramen compromise was defined as an abnormal narrowing of the neural foramen [11]. ≤12-mm anteroposterior diameter of the lumbar spinal canal is used as the cutoff [12]. Statistical Package for Social Sciences (SPSS) 26.0 version was used for data processing and analysis. Continuous variables were presented as mean ± standard deviation and categorical data were presented as frequency and percentages. Statistical correlation between the MRI Findings and patients’ demography and clinical observations was done using the kappa Coefficient. A Kappa Coefficient value of 0.5 and above was used as a good agreement at 95% level of significance i.e. P value < 0.05 was considered statistically significant.
- RESULTS & DISCUSSION
The mean age was 53.98 ± 13.065 years, the maximum incidence of backache was in the 5th decade of life (35.08%)
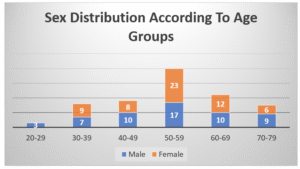
Figure 01: Age Distribution
Among the 114 cases studied, 56 (49.12%) were males and 58 (50.88%) were females.
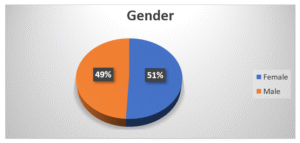
Figure 02: Gender Distribution
Out of the 114 cases studied, radicular pain along a specific dermatome was present in 51 patients (44.73%).
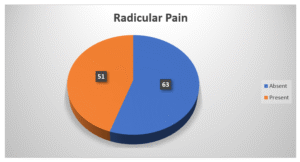
Figure 03: Radicular Pain
Straight leg raising test (SLRT) was positive in 91 patients (79.82%) and negative in 23 patients (20.18%).
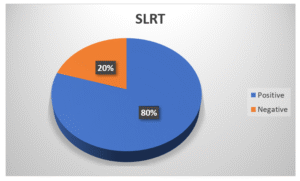
Figure 04: Straight Leg Raise Test
Ankle reflex was present in 78 patients (68.4%) and absent in 36 patients (31.6%).
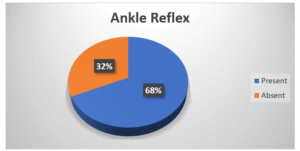
Figure 05: Ankle Reflex
Out of 114 patients, 40 patients (35.55%) had neurological deficits.
Out of 40 patients:
- 5(12.5%) patients had a neural deficit of S1 level.
- 3 (7.5%) patients had L4 and L5 level
- 25 (62.5%) patients had L5 and S1 level deficits.
7 (17.5%) patients had multiple-level involvement.
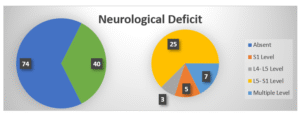
Figure 06: Neurological Deficit
There were 225-disc herniation in 114 patients studied
- Disc bulges were noticed in 83 levels (in 63 patients).
- Disc protrusion was noticed in 93 levels (in 73 patients)
- Disc extrusion was noticed in 49 levels (in 46 patients).
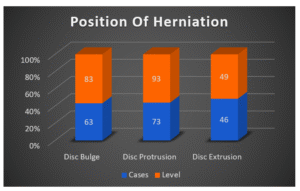
Figure 07: Position of Herniation
Out of 225 levels of disc herniation, position of the Protrusion (93 levels), extrusion (49 levels) was specified in the MRI, but not of disc bulge (83 levels). Thus, 142 different positions of the disc herniation (protrusion and extrusion) were found.
- 51 (35.92%) were central disc herniation (41 protrusion and 10 extrusion)
- 91 (64.08%) were paracentral (53 protrusion and 38 extrusion).
Neural Foramen compromise due to disc herniation was evident in 59 patients (51.11%) at 82 different disc levels.
- L3-L4 level: 11 patients
- L4-L5 levels: 46 patients
- L5-S1 levels: 25 patients
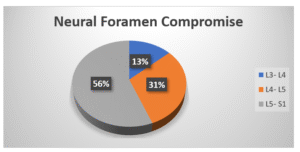
Figure 08: Neural Foramen Compromise
Nerve Root Compression was seen in 106 patients in 108 levels.
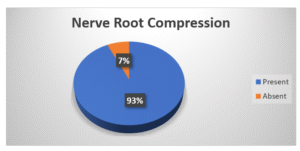
Figure 09: Nerve Root Compression
There was total 142 levels in 114 patients out of which
- 3 in L3 level
- 18 in L4 level
- 58 in L5 level
- 63 in S1 level
- 22 in 2-disc levels
- 3 in 3-disc levels
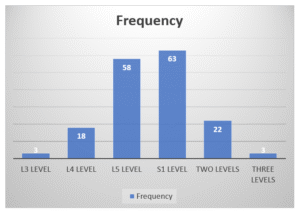
Figure 10: Frequency of MRI Level
Table 02: Correlation of Type of Herniation and Neurological Deficit
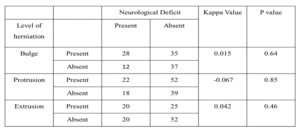
Table 03: Correlation of Neural Foramen Compromise in MRI and Clinical Findings
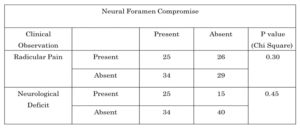
Table 04: Correlation of Nerve Root Compression in MRI and Clinical Findings
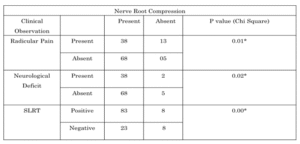
Table 05: Correlation of Nerve Root Compression at S1 and Absent Ankle Reflex
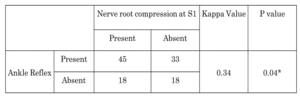
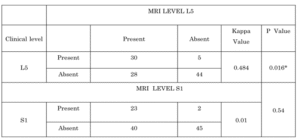
Table 06: Correlation between MRI Level S1, L5 and Clinical Level S1, L5 Respectively
DISCUSSION
The mean age in this study was 53.25 ± 12.90 years. There was slight female predominance with female 58 and male 56. The most common age group was 50-59 years, 40 (35.09%). The mean age of our study is similar to the most of studies regarding lumbar disc herniation as intervertebral disc starts to degenerate after 2nd decade of life: Its hydration, proteoglycan and cell content gradually decreases. Fissuring and cracks occur in annulus fibrosus which is aggravated by the combination of lateral bending, flexion and axial rotation forces that cause tear in this degenerated annulus. This might be the cause for the herniation being more common at 4th and 5th decade of life. After 60 years of age, as water content decreases, disc is desiccated and cells are replaced by granular cells which makes herniation less likely. Annular fibers are thus replaced with fibrous elements that are less elastic and it becomes stiffer and more resistant to deformation. In our study, out of 114 patients, radicular pain was present in 51(44.74%) patients and absent in 63 (55.26%) patients. The average duration of radicular pain was 8.74 months. The findings were similar with [13]; [14]. In our study, there was 118 different dermatomal level of pain in 91 patients. Out of these, 64 patients (70%) had pain distribution in the L5 dermatomal level (making it the commonest dermatome level involved) and 45 patients had pain distribution in the S1 dermatomal level (second commonest). The findings are in agreement with the study of Spangfort EV, 1972 who found that the levels L5 and S1 are responsible for over 95% (50% and 46% respectively) of herniation. A positive SLRT is a very important clinical sign for lower lumbar root tension. Multiple studies have corroborated the accuracy of the test and have noted positivity in 58% to 98% of the patients [15-18] with high sensitivity (pooled estimate 0.92, 95% CI: 0.87 to 0.95) and varying specificity (0.10 to 1.00, pooled estimate 0.28, 95% CI: 0.18 to 0.40). While its importance is highly appreciated, its absence does not preclude the presence of a lumbar disc herniation [18]. In this study, a positive SLRT was observed in 91 (79.82%) of our patients, which is in accordance to the studies [19], [20] who observed SLRT positive in 82.5%, 91.5% and 94% cases respectively. In our study out of 106 patients with nerve root compression in MRI, 83 had positive SLRT (78.30%). The correlation was statistically significant which is similar to the findings of [21] (90%) and Rasool F et al (47.1%). Both the studies have reported strong correlation of SLRT and Nerve root compression. Out of 225-disc herniation level (in 114 patients), disc bulge was noticed in 83 levels (in 63 patients), disc protrusion was noticed in 93 levels (in 73 patients) and disc extrusion was noticed in 49 levels (in 46 patients). We found no significant correlation between type of herniation and clinical findings. Our findings were in accordance with the findings of [22] (56 Disc Herniation in 50 patients) and [23] (72 Disc herniation in 60 patients) which could have been occurred due to incorrect explorations of the discs as the findings were relied on single observer and also, we have not performed correlation with a pre-operative MR and intraoperative findings. 40(35.09%) patients had neurological deficits in our study. Out of these, 15 (37.50%) patients had both motor and sensory deficits, 17 (42.50%) had only motor deficits and 8 (20%) have only sensory deficit. In our study, 5(12.5%) patients had a neural deficit of S1 level, 3 (7.5%) patients had L4 and L5 level, 25 (62.5%) patients had L5 and S1 level deficit whereas 7 (17.5%) patients had multiple levels involvement. In the study by Janardhan AP et al, out of 36 patients who had neurologic deficit, 20 (55.5%) patients had both motor and sensory deficit, 13(36.1%) had only sensory deficit and 12 had deficits involving more than one level. 2,16 and 6 patients had a neural deficit of L4, L5 and S1 level respectively. Rehman L et al observed 20 (40%) patients had only decreased sensations in S1 dermatome and 19 (38%) patients had decreased pin prick sensation in L5-S1dermatome. Rasool F et al also observed motor involvement in 34(85%) cases and sensory involvement in 31(77.5%) cases. There were 59 patients with neural foramen compromise, 51 patients (86.44%) had radicular pain with kappa value -0.020 (p –value = 0.002) and 40 (67.79%) had neurological deficit during clinical examination with kappa value -0.030 (p –value =0.030) which is statistically significant. In a similar study, [24] observed neural foramen compromise at 157 levels out of 290 levels of disc herniation in 119 patients and suggested an odd of 6.03; p<0.001 for developing neurologic symptoms in patients with neural foramen compromise. Our findings were similar to the findings of [25] who observed mean foramen compromise of 63.5% in the neuro deficit group and [26] who also observed greater mean compromise of the spinal canal significantly correlated with poorer outcome in patients with lumbar disc. In our study, out of 106 patients with nerve root compression 51 patients (48.11%) had radicular pain with kappa value 0.14 (p value = 0.036), which is statistically significant and 40 (37.74%) had neurological deficit during examination with kappa value 0.418 p value =0.019) which is also statistically significant. In a pioneer study in this field, [27] found the nerve root compression in patients with neurologic deficits was significantly higher than in those who were neurologically intact patients. (P, 0.05). In a similar study, [28] observed 36 patients with neurological deficits out of which 23 patients (63.88%) had nerve root compression seen in MRI and reported strong evidence of nerve root compression seen in MRI and clinical symptoms (P<0.001). Out of 63 patients with MRI showing nerve root compression at S1, 36 (57.14%) had absent ankle reflex with kappa value 0.35 (p value = 0.008), which is statistically significant. The findings are similar to the findings of [29] who in his study observed that out of 87 patients with nerve compression at S1, 73 (84%) had absent or decreased ankle reflex. An author [30] also reported strong association between an abnormality in ankle reflex and subjects with S1 Radiculopathy. The authors suggested that individuals with decreased ankle reflex were more than eight times more likely to have S1 radiculopathy than those with a normal reflex. In our study, out of 35 patients with MRI level L5, 30 patients had clinical level L5 which is statistically significant (kappa value 0.396, p value = 0.0023) and out of 63 patients with MRI level S1, 23 patients had clinical level S1 which is statistically significant (kappa = 0.510, p value = 0.02*). Our Findings were similar to the study by [31] who found strong correlation between clinical level and MRI level, the kappa value of statistical significance between them was 0.8. Similarly in study by Rehman L et al in case of L4-L5 level disc herniation, the sensitivity of all clinical features was 92% and positive predictive value was 95.8% while the specificity was 96% and negative predictive value was 88.46%. The chi square value was 38.78 with p value of 0.00 and in case of L5-S1 level disc herniation, the sensitivity and specificity of clinical features as a whole were 93.3% and 70% respectively. The positive predictive value was 82.3% with chi square value of 22.12 and p value of 0.000.
- CONCLUSIONS
Out of 114 patients, 56 (49.12%) were males and 58 (60.88%) were females. The mean age was 53.98 ± 13.065 years (range 21-79 years). Radicular pain along a specific dermatome was present in 51 patients (44.73%). There were 66 different dermatomal levels of pain in 51 patients out of which 36 were L5 (54.54%); 25 were S1 (37.88%) and 5 (7.58%) were L4. Straight Leg Raising Test (SLRT) was positive in 91 patients (79.82%), the neurological deficit was present in 40 patients (35.08%), and ankle jerk was absent in 36 patients (31.6%). Discussing MRI findings, out of 225-disc herniation levels, the most common type was disc protrusion (93, 41.33%), and levels being L4-L5 and L5-S1. There was a statistically significant correlation between MRI findings of Nerve Root compression and radicular pain (p-value = 0.01), neurological deficit (p-value = 0.02), and SLRT (p-value =0.00). Absent Ankle jerk and nerve root compression at S1 Level in MRI also correlated significantly (p value= 0.04). Clinical findings at L5 correlated significantly (p-value =0.016) with MRI Level at L5. There was no statistically significant correlation between types of disc herniation, neural foramen compromise, and MRI level S1 with Neurological deficit; Radicular pain and neurological deficit; and clinical level S1 respectively (p-value>0.05). There was no correlation between Clinical parameters (radicular pain, neurological deficit; motor and sensory; and absent ankle jerk) and MRI findings of disc herniation and neural foramen compromise. The most common levels of MRI were L5 and S1; with a significant correlation of Radicular Pain, SLRT, Neurological deficit (motor and sensory) and absent ankle jerk with the Nerve root compression seen in L5 but not in S1.
REFERENCES
- Hoy D, Bain C, Williams G, March L, Brooks P, Blyth F, Woolf A, Vos T, Buchbinder R. A systematic review of the global prevalence of low back pain. Arthritis & Rheumatism. 2012 Jun;64(6):2028-37.
- Sharma R, Tiwari A, Dwivedi R. Pattern of Lumbar MRI Changes in Patients with Chronic Low Back Pain in a Tertiary Care Centre .Journal of Lumbini Medical College. 2018;6(2):5 pages.
- Truumees E. A history of lumbar disc herniation from Hippocrates to the 1990s. Clin Orthop Relat Res. 2015 Jun;473(6):1885-95.
- Mixter W, Barr J. Rupture of the intervertebral disc with involvement of the spinal canal. N Engl J Med. 1934;211:210–215.
- Amin RM, Andrade NS, Neuman BJ. Lumbar Disc Herniation. Curr Rev Musculoskelet Med. 2017 Dec;10(4):507-516.
- Benzakour T, Igoumenou V, Mavrogenis AF, Benzakour A. Current concepts for lumbar disc herniation. International orthopaedics. 2019 Apr 4;43(4):841-51.
- Gadjradj PS, Arts MP, van Tulder MW, Rietdijk WJR, Peul WC, Harhangi BS (2017) Management of symptomatic lumbar disk herniation: an international perspective. Spine 42(23):1826–1834
- Sorensen SJ, Kjaer P, Jensen ST, Andersen P. Low-field magnetic resonance imaging of the lumbar spine: reliability of qualitative evaluation of disc and muscle parameters. Acta Radiologica. 2006 Nov;47(9):947-53.
- Dipesh Pariyar, Rishi Bista & Rajaram Maharjan (2024). Ankle Brace V/s below Knee Slab in Lateral Ankle Sprains (Grade I and II). Dinkum Journal of Medical Innovations, 3(11):750-760.
- Beattie PF, Meyers SP, Stratford P, Millard RW, Hollenberg GM. Associations between patient report of symptoms and anatomic impairment visible on lumbar magnetic resonance imaging. Spine (Phila Pa 1976). 2000; 25:819-28.
- Borenstein DG, O’Mara JW Jr, Boden SD, Lauerman WC, Jacobson A, Platenberg C et al. The value of magnetic resonance imaging of the lumbar spine to predict low-back pain in asymptomatic subjects: A sevenyear follow-up study. J Bone Joint Surg Am. 2001; 83:1306-11.
- Donnally CJI, Dulebohn SC (2017) Lumbar degenerative disk disease, https://www.ncbi.nlm.nih.gov/books/NBK448134, Accessed 8 December 2021
- Walmsley R. The development and growth of the intervertebral disc. Edinburgh medical journal. 1953 Aug;60(8):341.
- Ebraheim NA, Hassan A, Lee M, Xu R. Functional anatomy of the lumbar spine. InSeminars in pain medicine 2004 Sep 1 (Vol. 2, No. 3, pp. 131-137). WB Saunders.
- Nedresky D, Reddy V, Singh G. Anatomy, Back, Nucleus Pulposus. In: StatPearls. StatPearls Publishing, Treasure Island (FL); 2020
- Nosikova YS, Santerre JP, Grynpas M, Gibson G, Kandel RA. Characterization of the annulus fibrosus-vertebral body interface: identification of new structural features. J Anat. 2012 Dec;221(6):577-89.
- Moore RJ. The vertebral endplate: disc degeneration, disc regeneration. Eur Spine J. 2006 Aug;15 Suppl 3(Suppl 3):S333-7. Coventry MB. Anatomy of the Intervertebral Disk.Clin Orthop Relat Res. 1969;67:9-15.
- Coventry MB. Anatomy of the Intervertebral Disk.Clin Orthop Relat Res. 1969;67:9-15.
- Klein JD, Garfin SR. Clinical evaluation of patients with suspected spine problems. In: Frymoyer JW, ed. The adult spine. 2d ed. Philadelphia: Lippincott-Raven, 1997:319–40.
- Humphreys SC, Eck JC. Clinical evaluation and treatment options for herniated lumbar disc. American family physician. 1999 Feb 1;59(3):575
- Waddell G, Somerville D, Henderson I, Newton M. Objective clinical evaluation of physical impairment in chronic low back pain. Spine. 1992;17:617–28.
- Beattie P. The relationship between symptoms and abnormal magnetic resonance images of lumbar intervertebral disks. Physical therapy. 1996 Jun 1;76(6):601-8.
- Janardhana AP, Rao S, Kamath A. Correlation between clinical features and magnetic resonance imaging findings in lumbar disc prolapse. Indian journal of orthopaedics. 2010 Jun;44(3):263-9.
- Jain S, Kumar S. Correlation between clinical features and magnetic resonance imaging findings in lumbar disc prolapse. Indian journal of orthopaedics. 2011 Mar;45(2):105.
- Dutta S, Bhave A, Patil S. Correlation of 1.5 Tesla magnetic resonance imaging with clinical and intraoperative findings for lumbar disc herniation. Asian spine journal. 2016 Dec;10(6):1115.
- Thapa SS, Lakhey RB, Sharma P, Pokhrel RK. Correlation between clinical features and magnetic resonance imaging findings in lumbar disc prolapse. Journal of Nepal Health Research Council. 2016 Nov 16.
- Sarkar MK, Kundu PK, Alahi MM, Amin MP, Mallick AK, Ahmed Q, Kafiluddin M. Correlation Between Clinical And Magnetic Resonance Imaging Findings In Patients With Lumbosacral Radiculopathy. TAJ: Journal of Teachers Association. 2015;28(1):32-9.
- Rijal A, Paudel M. Correlation between Clinical Features and Findings Observed on Magnetic Resonance Imaging in Patients with Lumbar Disc Prolapse. Asian Journal of Orthopaedic Research. 2020 Jan 24:26-33.
- Yousif S, Musa A, Ahmed A, Abdelhai A. Correlation between findings in physical examination, magnetic resonance imaging, and nerve conduction studies in lumbosacral radiculopathy caused by lumbar intervertebral disc herniation. Advances in orthopedics. 2020 Jan 24;2020.
- D Hoy, P Brooks, F Blyth, R Buchbinder. The Epidemiology of low back pain Clinical rheumatologyDec;24(6):769-81.
- Steurer J, Roner S, Gnannt R, Holder J. Quantitative radiologic criteria for the diagnosis of lumbar spinal stenosis: a systematic literature review BMC Musculoskeletal Disorders, 2011; 12: 175.
Publication History
Submitted: July 08, 2025
Accepted: July 28, 2025
Published: July 31, 2025
Identification
D-0450
DOI
https://doi.org/10.71017/djmi.4.7.d-0450
Citation
Krishna Bahadur Bista, Bhupendra Man Singh Shrestha & Bodh Raj Gautam (2025). To Find Out the Correlation between Clinical Features and MRI Findings in Cases of Lumbar Disc Prolapse. Dinkum Journal of Medical Innovations, 4(07):426-439.
Copyright
© 2025 The Author(s).


