Publication History
Submitted: February 16, 2025
Accepted: March 02, 2025
Published: March 31, 2025
Identification
D-0417
DOI
https://doi.org/10.71017/djmi.4.3.d-0417
Citation
Nabin Thapa Magar, Manish Adhikari, Swagat Khadka & Mahendra Acharya (2025). Drug Utilization Pattern of COPD in KANKAI Municipal Hospital, KANKAIN Municipality, JHAPA. Dinkum Journal of Medical Innovations, 4(03):136-146.
Copyright
© 2025 The Author(s).
136-146
Drug Utilization Pattern of COPD in KANKAI Municipal Hospital, KANKAIN Municipality, JHAPAOriginal Article
Nabin Thapa Magar 1*, Manish Adhikari 2, Swagat Khadka 3, Mahendra Acharya 4
- Assistant Professor, Purbanchal University School of Health Sciences, Morang, Nepal.
- Purbanchal University School of Health Sciences, Morang, Nepal.
- Purbanchal University School of Health Sciences, Morang, Nepal.
- Purbanchal University School of Health Sciences, Morang, Nepal.
* Correspondence: phrnabin888@gmail.com
Abstract: Chronic Obstructive Pulmonary Disease (COPD) is a major cause of severe illness and death globally, especially in resource-poor settings. Drug utilization pattern provides knowledge about how drugs are used which is important to improve the results of therapy and guarantee appropriate use of drugs. This study assessed the drug utilization pattern of COPD in KANKAI Municipal Hospital, KANKAI Municipality in JHAPA district. It used a hospital facility based descriptive cross-sectional study. The study area was KANKAI Municipal Hospital, KANKAI Municipality, JHAPA District of Koshi Province, Nepal. It was conducted among the COPD patients visiting the outpatient department of KANKAI Municipal Hospital.This study used existing data to determine the utilization pattern of COPD drugs. A patient profile form was used to collect the data on drug utilization pattern. Validity and reliability were maintained by consulting the research supervisor, concerned authority and colleagues. Out of the 151 prescriptions analyzed, females (53.6%) were slightly higher than males (46.4%) with mean age of 71.04±12.26 years. Out of (80.1%) with comorbidities, the most common one was hypertension (24%). Inhalational route (69.8%) was the common route of administration of drugs in most of the cases followed by the oral route (30.2%). The most frequently prescribed class of drugs were bronchodilator (91.4%) followed by inhaled corticosteroids (84.1%). Antibiotics were prescribed in (22.5%) of the cases. (85.4%) of the patients were prescribed combination therapy. The drug utilization pattern for COPD in the hospital setting reveals significant insights into the management practices and therapeutic strategies employed. Our study highlighted the predominant use of bronchodilators, including both short-acting and long-acting agents, as the cornerstone of COPD treatment, reflecting adherence to established clinical guidelines.
Keywords: chronic obstructive pulmonary disease, drug utilization, pattern, antibiotics
- INTRODUCTION
Non-communicable diseases (NCDs) are the primary cause of mortality in Nepal. These diseases mostly include diabetes, cancer, chronic respiratory conditions, and cardiovascular diseases. Indirect estimates place the number of NCD-related deaths in 2016 at over 127 thousand, accounting for 66% of all deaths in the country. Over time, Nepal’s NCD burden has increased, necessitating immediate action to prevent and control NCDs.[1] Chronic obstructive pulmonary disease (COPD) is a chronic inflammatory lung disease that results in blocked airflow from the lungs. Symptoms include difficulty breathing, coughing, sputum production, and wheezing. It is usually caused by prolonged exposure to irritating chemicals or particulate particles, most commonly from cigarette smoke. People with COPD are more likely to develop heart disease, lung cancer, and other illnesses. Emphysema and chronic bronchitis are the two most frequent diseases that cause COPD. These two diseases are frequently present together and can vary in severity among COPD patients. Chronic bronchitis is an inflammation of the bronchial tube linings that transport air to and from the lungs’ air sacs (alveoli). It is distinguished by daily coughing and mucous (sputum).[2] The World Health Organization (WHO) described drug utilization study as “the marketing, distribution, prescription, and use of drugs in a society, with special emphasis on the resulting medical, social, and economic consequences” in 1977.Facilitating the reasonable use of medications in communities is the main goal of drug use research. For each patient, rational drug usage means a prescription for a well-researched medication at the right dosage, with the right information, and at a reasonable cost. Without understanding how medications are given and used, it is challenging to start a conversation about responsible drug use or to recommend changes to prescription practices.[3]Drug use analysis can minimize overall healthcare expenses by improving treatment outcomes, minimizing adverse drug reactions, and reducing wasteful pharmaceutical spending. [4] COPD deteriorates without therapy. Furthermore, there may be an increased risk of having some chronic health concerns as a result. People with COPD may stop exercising owing to dyspnea, increasing their risk of acquiring other illnesses such as high blood pressure, heart disease, obesity, and diabetes.[5]Bronchodilators such selective β2-adrenergic agonists (short- and long-acting), anticholinergics, theophylline, or a combination of these drugs are commonly utilized. Patients with stable mild to severe COPD are frequently recommended not to take glucocorticoids due to their high cost, lack of efficacy, and side effects. Glucocorticoids are recommended in patients of severe COPD and recurring exacerbations. Because the current COPD treatment is inadequate, new pharmacological approaches must be developed [6]. The main goal of COPD treatment is to use bronchodilators to relax the smooth muscle in the airways. There hasn’t been much success with use of PDE inhibitors, like theophylline, and inhaled corticosteroids to lessen inflammation. Nonpharmacologic therapy includes lung rehabilitation, smoking cessation, and long-term oxygen therapy (LTOT) [7].The outcomes of irrational prescribing have a detrimental effect on people’s health and the economics of society as a whole, wasting money and creating numerous health risks [8]. With 3.23 million deaths from chronic obstructive pulmonary disease (COPD) in 2019, it ranks as the third most common cause of mortality globally. Almost 90% of COPD-related fatalities in people under 70 happen in low- and middle-income nations (LMIC). When evaluating the world’s healthiest countries based on disability-adjusted life years, COPD ranks eighth. In high-income nations, tobacco use is the primary cause of COPD cases more than 70%. 30 to 40 percent of COPD cases in LMICs are caused by tobacco use, and one important risk factor is indoor air pollution.[9]Overuse of medications is a significant issue on a global scale. According to WHO estimates, half of patients do not take their medications as recommended and over half of all medications are improperly marketed, administered, or prescribed. Misuse, abuse, or overuse of medications wastes limited resources and poses a public health risk [10].Pakistan ranks among the nations with the largest number of prescriptions filled because of the overuse of injectable medicines and antibiotics. This is because doctors are largely motivated by the lucrative financial incentives of pharmaceutical firms rather than by clinical results, which leads to a lack of ethical procedures in prescription. Over the past several years, there has been a noticeable increase in this unethical conduct, which is still a problem in Pakistan. There isn’t currently a code of ethics for pharmaceutical businesses’ marketing and promotional efforts[11]. The increasing cases of COPD in Nepal may also be due to improper management of the disease and medication non adherence. Low socio-economic status, Illiteracy and negligence may be the main factors for medication non adherence in context of Nepal. Nepalese women are particularly vulnerable to developing COPD as a result of indoor air pollution because nearly 85% of households still rely on biofuels like wood and other materials to cook their meals. Our people’s low level of health literacy when compared to those in rich western nations exacerbates the situation[12]. The prevalence of COPD is gradually increasing in Nepal according to different researches conducted in recent times. This is conducted to study the drug utilization of COPD in a secondary care hospital setting in Nepal. The study in drug utilization pattern may help in different ways to improve the present status of the disease. Drug utilization helps in studying the severity of disease in the country. Analyzing the utilization pattern of drug may be helpful findings gaps in the treatment that optimizes the pharmacotherapy of COPD. Analyzing medication use helps patient to yield information for cost-effectiveness evaluations of treatment options of COPD in Nepal. Irritational prescribing may affect the health of the patients. So, drug utilization studies help in determining if the therapies are rationale and comply with national or international guidelines. Drug utilization research was defined by WHO in 1977 as “the marketing, distribution, prescription, and use of drugs in a society, with special emphasis on the resulting medical, social and economic consequences’’.[3]The use of pharmaceuticals in medicine has increased significantly within the past 50 years.[13]A diverse range of descriptive and analytical techniques are combined in drug utilization research to quantify, comprehend, and assess the processes involved in the prescription, dispensing, and consumption of medications[14]. Drug utilization studies look into the prescription, dispensing, and/or usage of medications in routine clinical settings[17]. Various studies have been conducted to assess the drug utilization pattern of COPD. Various medications used in COPD was observed in these studies. With 3.23 million fatalities from chronic obstructive pulmonary disease (COPD) in 2019, it ranks as the third most common cause of mortality globally. In high-income nations, tobacco use is the primary cause of COPD cases more than 70%. 30 to 40 percent of COPD cases in LMICs are caused by tobacco use, and one important risk factor is indoor air pollution [18]. Treating chronic obstructive pulmonary disease (COPD) using inhalers involves a range of innovative single-, dual, and triple-therapy options. These inhalers might include inhaled corticosteroids, short-acting or long-acting beta2 agonists, short-acting or long-acting muscarinic antagonists, or both [19]. Various studies show that bronchodilators are the most prescribed class of drugs in COPD and more efficient in the treatment of COPD than other class of drugs.
- MATERIALS & METHOD
This study achieved drug utilization pattern of COPD patients in KANKAI Municipal Hospital which is located in JHAPA district. This study was based on quantitative research method. The study was carried in Municipal hospital of KANKAI Municipality, JHAPA. The study design was hospital based descriptive cross-sectional study. The Study was conducted in outpatient Department of KANKAI Municipal Hospital located in KANKAI Municipality, JHAPA district of Nepal. KANKAI municipality has occupied 79.1 sq.km which is about 58km far from Purbanchal University School of health science (PUSHS). The hospital has different inpatient and outpatient department. The study population for this study was COPD patients aged 21 above visiting the outpatient department of KANKAI Municipal Hospital. In order to draw accurate and representative information from the sample, probability sampling technique was applied for this study. Simple random was used. Initially, information on the patients of a 60 days period was obtained from the hospital records. Then, the study participants were selected by using computer generated random number table method until the fulfilment of sample size.
Sample size calculation (n) = 𝒁2 ×𝒑×𝒒/𝒅²
Where, Z = 1.96 for 5% level of significance
Probability of drug utilization pattern (P) = 0.11 (obtained from this previous study.)[20]
q= (1-p) =1-0.11=0.89
Allowable error (d) =5% Now, n= 𝑍2×𝑝×𝑞/𝑑²
n= (1.96) ²× (0.11) × (0.89) / (0.05) ² =150.43 151
The total sample size for the study is 151.
This study used existing data to determine the drug utilization pattern of COPD drugs. The data on patients was obtained from the records existing in the Hospital either electronic or physical records. Then the records were reviewed to obtain the necessary information. A patient profile form was used to collect the data on drug utilization pattern. The tool was self-constructed by taking references from various studies according to context of the study. For this, formal consent was obtained from the respective authors. After getting ethical clearance from the review committee of PUSHS, and an approval letter from KANKAI Municipal Hospital, the data collection process was commenced. The data was obtained by keeping a 2 months period of patients visiting the Hospital. For maintaining the reliability of the study, pre-testing was done on 10% i.e. (16) of the total sample population. In order to ensure that the tool was applicable, the pre testing was done on population other than the selected sample population. Following the data collection, IBM SPSS version 20 was used for data entry and analysis. Descriptive statistics was used for summarizing the data and the results was presented using frequency tables, mean, standard deviation and percentage. Validity of the research was maintained by consulting the research supervisor, concerned authority and colleagues. Representative population was selected by setting the standard inclusion criteria. Reliability of the research was maintained by pre-testing the tool in a hospital that is homogeneous to the study hospital. Close monitoring and supervision from the supervisor also helped maintaining the validity and reliability of the research. The study secured ethical clearance from ethical committee of PUSHS. Approval letter from hospital was taken before conducting the study. Confidentiality of participants identity was maintained.
- RESULTS & DISCUSSION
During this study a total of 151 prescriptions were analyzed and collected. Table 01 presents the socio-demographic characteristics of the patients. Among the 151 patients, females (53.6%) were slightly higher than males (46.4%). The patients were divided into four age groups in which (64.9%) belonged to the age group (61 to 80) which was the highest, followed by (19.2%) belonged to the age group 81 above. The mean age of the respondents was 71.04±12.26 years.
Table 01: Socio-demographic characteristics of the respondents
| Characteristics | Frequency | Percentage (%) |
| Gender | ||
| Male | 70 | 46.4 |
| Female | 81 | 53.6 |
| Age (Years) | ||
| 21-40 | 4 | 2.6 |
| 41-60 | 20 | 13.2 |
| 61-80 | 98 | 64.9 |
| 80 above | 29 | 19.2 |
Figure 01 represents that Inhalational route (69.8%) was the common route of administration of drugs in most of the cases followed by the oral route (30.2%) was the second most common route.
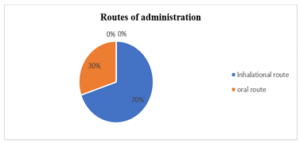
Figure 01: Routes of administration
Figure 02 represents classes of drugs prescribed. Bronchodilators (91.4%) were the most prescribed class of drugs followed by inhaled corticosteroids (84.1%). Oral corticosteroids (38.4%) were prescribed followed by leukotriene antagonists (21.3%) followed by antihistamine (23.2%). Antibiotics were prescribed in (22.5%) of the cases.
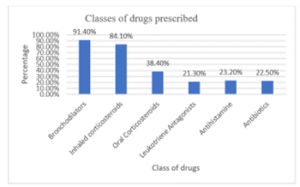
Figure 02: Classes of drug prescribed
Table 02 represents that Formoterol (64.2%) was the most prescribed bronchodilator which was used in combination. Tiotropium bromide (53%) was the second most prescribed bronchodilator followed by Salmeterol (20.5%) followed by Salbutamol (14.6%) was prescribed.
Table 02: Bronchodilators prescribed
| Drugs | Frequency | Percentage (%) |
| Beta-2 Sympathomimetics | ||
| Formoterol | 97 | 64.2 |
| Salmeterol | 31 | 20.5 |
| Salbutamol | 22 | 14.6 |
| Anticholinergics | ||
| Tiotropium Bromide | 80 | 53 |
| Methylxanthines | ||
| Doxophylline | 27 | 17.9 |
Table 03 represents that Budesonide (64.2%) was the most prescribed Inhaled corticosteroids followed by Fluticasone (20.5%) which was mostly used in combination.
Table 03: Inhaled corticosteroids prescribed
| Drugs | Frequency | Percentage (%) |
| Inhaled corticosteroids | ||
| Budesonide | 97 | 64.2 |
| Fluticasone | 31 | 20.5 |
Oral corticosteroids were the third most prescribed class of drugs. Prednisolone was prescribed (38.4%) which was the only oral corticosteroids prescribed. Table 04 represents that Montelukast (22.5%) was prescribed which was the only Leukotriene antagonists. Antihistamines like levocetirizine were prescribed in (23.2%) of the cases.
Table 04: Leukotriene antagonists and antihistamine prescribed
| Drugs | Frequency | Percentage (%) |
| Leukotriene antagonists | ||
| Montelukast | 32 | 21.2 |
| Antihistamine | ||
| Levocetirizine | 31 | 20.5 |
Table 05 represents by amoxicillin (32.35%) was the most prescribed antibiotics followed by Azithromycin (14.7%). Antibiotics were prescribed in (22.5%) of the cases.
Table 05: Antibiotics prescribed
| Drugs | Frequency | Percentage (%) |
| Antibiotics | ||
| Amoxicillin | 11 | 32.35 |
| Azithromycin | 5 | 14.7 |
Table 06 represents that majority of the patients (85.4%) were given combination therapy. Bronchodilators like Formoterol, Salmeterol and Inhaled corticosteroids like Budesonide, Fluticasone were mostly used in combination. Formoterol and Budesonide combination (64.2%) was mostly prescribed followed by Salmeterol and Fluticasone (20.5%).
Table 06: Combination therapy prescribed
| Drugs | Frequency | Percentage (%) |
| Combination Therapy | ||
| Formoterol and Budesonide | 97 | 64.2 |
| Salmeterol and Fluticasone | 31 | 20.5 |
Table 07 represents that the (80.1%) patients were suffering from co-morbidity. Hypertension (24%) was the most common comorbidity followed by Diabetes mellitus (19.1%). Other conditions: include hypothyroidism, anaemia, anxiety, Hypocalcaemia, hyperuricaemia, asthma, UTI, allergic rhinitis, Osteoarthritis, Community acquired pneumonia, coronary artery diseases.
Table 07: Comorbid conditions of respondents
| Characteristics | Frequency | Percentage (%) |
| Comorbidity | ||
| Hypertension | 59 | 24 |
| Diabetes mellitus | 47 | 19.1 |
| Vitamin deficiency | 26 | 10.6 |
| URTI | 21 | 8.5 |
| DLP | 21 | 8.5 |
| Peripheral neuropathy | 20 | 8.1 |
| BPH | 15 | 6.1 |
| Others | 37 | 15 |
DISCUSSION
In this study, females (53.6%) were found to be higher than males (46.4%). Similar studies conducted by Gaviria Mendoza in Colombia, by Lee CH in South Korea and by Arya Gigi in Bangalore, India found that the percentage of males were higher than females i.e. (50.1% males, 49.9% females),(73% males and 27% females) and (78% males and 22% females)respectively which was not similar to this study.[21,22,29] The high prevalence of COPD in females maybe due to the domestic smoke exposure as it is one of the main risk factors of COPD in Nepal. In this study, the maximum patients were from the age group (61-80). Similar studies conducted by Gaviria Mendoza in Colombia, by Unni PVS in Kerala, India and by Bajracharya M in Lalitpur, Nepal also found that the maximum patients were from the age group (61-80) i.e. (71-80), (61-70) and (70-79) respectively.[21,27,31]. The findings of this study show that the inhalational route (69.8%) was the most common route than oral route (30.2%). Similar studies conducted by M Aktar in Bangladesh, by Unni PVS in Kerala India and Arya Gigi in Bangalore found that most preferred route was Oral (34.12%), Parenteral (47.06%) and Oral (44.5%) respectively.[24,27,29]This difference in finding may be due to the fact that these two studies have been conducted in two different countries and even the cities are different between the two studies. The key findings of this study showed that Bronchodilators (91.4%) was the most prescribed class of drugs. Similar studies conducted by Unni PVS in Kerala India and M Aktar in Bangladesh also found that bronchodilators were the most prescribed class of drugs i.e. (57.19%) and (98.30%) respectively[24,27]. The findings showed that Formoterol (64.2%) was the most prescribed bronchodilator. Similar studies conducted in Bangladesh and in Bhopal India also found that formoterol was the most prescribed bronchodilator i.e. (45.49%) and (80.5%) respectively [24,32]. However Tiotropium bromide (53%) was not the most prescribed anticholinergic drug in this findings which was not similar to study conducted by Dr Sachin Parmar in Bhopal, India which showed that Ipratropium bromide (48.61%) was the most prescribed anticholinergic drug followed by tiotropium bromide (34.72%) [32]. The findings of this study showed that Anticholinergics (53%) were prescribed more than methylxanthines (17.9%). Similar studies conducted by Shiv Kumar in Karnataka; India showed that Methylxanthines were prescribed more than anticholinergics which was not in accordance to this study [28]. In this study, it was found that Inhaled corticosteroids (84.1%) were the second most prescribed class of drugs. In contrast, a study conducted in Gurugram, India by Poonam Salwan showed that Inhaled corticosteroids was the most prescribed class of drugs i.e. (67.85%) [33]. Budesonide (64.2%) was the most prescribed Inhaled Corticosteroids. In contrast, a study conducted in India also showed that Budesonide was the most prescribed Inhaled corticosteroids which was prescribed to (63.5%) of the patients. In this study, fluticasone was prescribed to (20.5%). The study also showed that Fluticasone was prescribed to (21.5%) Which was quite similar [34]. This finding showed that Montelukast and Levocetirizine was prescribed in (21.2%) and (20.5%) of the patients. In contrast, a study conducted by Shalini Salwan in India showed that Montelukast and Levocetirizine was prescribed to (37.5%) and (32.14%) [33]. The difference in the findings due to fact that the study is conducted into two different cities of two different countries. This study showed that antibiotics was prescribed in (22.5%) of the cases. Similar study conducted by Sai Lakshmi Srikala T also showed that antibiotics was prescribed in (19.09%) which is quite similar to this study.[35] However, study conducted by Sunil S showed that antibiotics was prescribed in (42%) of patients and was the most prescribed class of drugs [36]. The findings of this study were not in accordance to this study. This may be an indicator of the prevalence of infections among the patients with acute exacerbation of COPD in different demographic areas. The key findings of this study showed that the majority (85.4%) of the patients were given combination therapy. In contrast, a study conducted by M Aktar in Bangladesh showed that combination therapy was prescribed to (90.48%) of the patients which was quite similar to our study.[24] This study showed that Formoterol and Salmeterol was prescribed in (64.2%) of the cases which was the most prescribed combination treatment. Similar study conducted by Sharon Sunil showed that Salbutamol+ Ipratropium bromide+ Budesonide (40%) was the most preferred combination which was not in accordance to this study [25]. This study reported that (80.1%) of the patients were suffering from co-morbid conditions. Similar study conducted by DB Jyothi and Shiv Kumar showed that co-morbid conditions was present in (78%) and (71.77%) respectively [28,34]. The key outcomes of this findings showed that hypertension (24%) was most common the co-morbid condition. In contrast, a study conducted by M Bajracharya in Nepal also showed that hypertension (38.5%) was the common co-morbid condition. This study showed diabetes mellitus was present in (19.1%) of the patients which was quite similar to study conducted by M Bajracharya i.e. (19%) [31]. The difference in findings of the different studies may be due to the fact that the studies were conducted in two different cities of two different nations, sample size of the studies, Unavailability of medications and economic status of the patients. The study likely reveals the drug utilization pattern of COPD patients in KANKAI Municipal Hospital. Common problems may include restricted availability to specific drugs, patient financial restrictions, and varied degrees of healthcare practitioner training. However, this study on drug utilization pattern of COPD highlights the need for customized healthcare, ensuring essential COPD medications available across all regions, enhancing the knowledge and practices of healthcare providers regarding COPD management, government and healthcare policies to support affordable and effective COPD treatment options.
- CONCLUSIONS
This study provides an insight on the current status of drug utilization pattern of COPD in KANKAI Municipal Hospital, JHAPA, Nepal. This study used existing data to determine the utilization pattern of COPD drugs. A patient profile form was used to collect the data on drug utilization pattern. Validity and reliability were maintained by consulting the research supervisor, concerned authority and colleagues. Out of the 151 prescriptions analyzed, females (53.6%) were slightly higher than males (46.4%) with mean age of 71.04±12.26 years. Out of (80.1%) with comorbidities, the most common one was hypertension (24%). Inhalational route (69.8%) was the common route of administration of drugs in most of the cases followed by the oral route (30.2%). The most frequently prescribed class of drugs were bronchodilator (91.4%) followed by inhaled corticosteroids (84.1%). Antibiotics were prescribed in (22.5%) of the cases. (85.4%) of the patients were prescribed combination therapy. The drug utilization pattern for COPD in the hospital setting reveals significant insights into the management practices and therapeutic strategies employed. Our study highlighted the predominant use of bronchodilators, including both short-acting and long-acting agents, as the cornerstone of COPD treatment, reflecting adherence to established clinical guidelines. This study was originated from the identified need that COPD is the most prevalent disease in Nepal according to various recent studies. The studies aimed at identifying the current trends of pattern of drugs in COPD, routes of administration of COPD drugs and co-morbid conditions of COPD patients. This study was successful in identifying the objectives of our study. The study of the pattern of drug utilization in the COPD patients of a Municipal Hospital is quite an informative dataset of the prescribing trend along with the patient demography. Findings of this study showed that most of the patients with COPD were old and a good percentage of them were between 61-80 years. The most predominant mode of administration of the drug is through the inhalational routes, and frequently prescribed drugs are bronchodilators and inhaled corticosteroids. The noteworthy findings are the widespread use of combination therapy, especially in the combination involving Formoterol and Budesonide, attesting to the complexity of managing COPD. Further to this point, it was noted that a significant percentage of patients had comorbid conditions with hypertension and diabetes mellitus being the most frequently encountered. Indeed, the results chime with the fact that therapeutic strategy in COPD needs to be tailored in relation to the age, comorbidities, and specific drug utilization patterns in the observed population.
- RECOMMENDATIONS
According to the study’s findings, future research and healthcare practice should therefore dwell on some main areas. The inhalation therapy which was predominantly used by about 69.8% should be emphasized, since it is associated with effective delivery of medications directly into the lungs and with a high level of compliance from patients especially in an elderly population. Extensive prescribing of bronchodilators in particular within combination therapies to the tune of 85.4 percent underlines the central role they play in the management of COPD. Therefore, an assessment of their long-term benefits against the risks of such combinations is important. Corticosteroids, whether inhaled or oral are also used significantly and hence it will be very essential to take note of anti-inflammatory action and related risks in continuous usage. Although antibiotic use was less common, it was noteworthy and would require careful review to avoid the development of resistance. Comorbidities were frequent, particularly hypertension and diabetes mellitus, which suggested that COPD patients gain as much from integrated management approaches for these conditions as they do for COPD itself. Finally, the less commonly prescribed the rapies leukotriene antagonists and antihistamines need further evaluation for their potential as alternative treatments. The recommendations made here are designed to improve the whole management of COPD in KANKAI Municipal Hospital making its treatment strategies effective and sustainable.
REFERENCES
- Diseases N communicable, Services H. Burden of Non-communicable Diseases in Nepal: An Urgent Need for Actions. 2017
- COPD. 2020.From: https://www.mayoclinic.org/diseases-conditions/copd/symptoms-causes
- Organization WH. Introduction to drug utilization research. 2003.
- Yadav A, Yadav BK, Chhetri P. drug utilization pattern and costanalysis of drugs used at COPD outpatient department in a tertiary care hospital. 2023;11(01).
- Welte T, Vogelmeier C, Papi A. review article copd : early diagnosis and treatment to slow disease progression. 2015;(March):336–49.
- Montuschi P. Pharmacological treatment of chronic obstructive pulmonary disease. 2006;1(4):409–23.
- Littner R. Michael, HDA. Sleep-Related Disorders in Chronic Pulmonary Disease. Sciencedirect. 2012
- Shamsur Rahman, David Matanjun, Urban John Arnold D’souza, Wan Salman Wan Saudi, Fairrul Kadir, Tan Teck Song, et al. Irrational Use of Drugs. Borneo Journal of Medical Sciences (BJMS). 2021;15(1):5.
- Manila Shrestha, Kalpana Sharma, Srijana Ghimire, Swarnima Maskey, Prakash Pariyar & Chandra Bahadur Sunar (2024). Missed Nursing Care at Tertiary Hospital, Bharatpur, Chitwan. Dinkum Journal of Medical Innovations, 3(10):716-732.
- World Health Organization. Promoting rational use of medicines2024. Available from: https://www.who.int/activities/promoting-rational-use-of-medicines
- Aslam F, Khan FU, Yang Y. Rational Prescription and Cost-Effective Medication: Challenges and Opportunities in Pakistan. Innov Pharm. 2020;11(4):1.
- clinic one,COPD – Overview, Causes, Symptoms and Treatment in Nepal. Available from: https://www.clinicone.com.np/copd-cases-in-nepal/
- Wades O, Lidos MR. the Concept of Drug Utilization Studies.1979;(8).
- Misra A. Drug utilization pattern in four major wards of a tertiary hospital in eastern Nepal. 2015;13(2):50–65.
- Mittal N, Mittal R, Singh I, Shafiq N, Malhotra S. Drug utilization study in a tertiary care center: Recommendations for improving hospital drug dispensing policies. Indian J Pharm Sci. 2014;76(4):308–14.
- Anisha Shrestha, Archana Pandey Bista, Kalpana Paudel & Madhusudan Subedi (2024). Experiences of Nurses Regarding Caring Behavior in Intensive Care Units. Dinkum Journal of Medical Innovations, 3(07):483-492.
- Mayal Stephen J. BA k. Pharmacovigilance planning. sciencedirect. 2014;137–61.
- Gama H. Drug utilization studies. Arquivos de Medicina. 2008;
- Brunner WM, Siddiqui N, Scribani MB, Krupa NL, Riesenfeld E. Prescribing Patterns for Long-Acting Inhaled Bronchodilators Among Rural Adults with Chronic Obstructive Pulmonary Disease. J Clin Med Res. 2022;14(9):388–93.
- Weiss TJ, Rosen Ramey D, Yang L, Liu X, Patel MJ, Rajpathak S, et al. Medication use by US patients with pulmonary hypertension associated with chronic obstructive pulmonary disease: a retrospective study of administrative data. BMC Pulm Med. 2022;22(1):1–10.
- Machado-Duque ME, Gaviria-Mendoza A, Valladales-Restrepo LF, González-Rangel A, Laucho-Contreras ME, Machado-Alba JE. Patterns and Trends in the Use of Medications for COPD Control in a Cohort of 9476 Colombian Patients, 2017–2019. International Journal of COPD. 2023; 18:1601–10.
- Lee CH, Kim MS, Yeo SH, Rhee CK, Park HW, Yang BR, et al. Treatment patterns and cost of exacerbations in patients with chronic obstructive pulmonary disease using multiple inhaler triple therapy in South Korea. Respir Res. 2022;23(1):1–13.
- Liao KM, Chiu KL, Chen CY. Prescription patterns in patients with chronic obstructive pulmonary disease and osteoporosis. International Journal of COPD. 2021; 16:761–9.
- M Aktar 1, A U Ahmed, F Sabrin, M S Rana, S S Rasna, K E Zannat, An Afrin, S Sultana, S Jahan, S Nahar RNS. Pattern of Prescribing Drugs in Chronic Obstructive Pulmonary Disease in a Tertiary Care Hospital of Bangladesh. pubmed. 2020;
- Rakesh Kumar Mahato, Sagar Pokharel & Avinash Sahani (2024). Knowledge & Practice Regarding Neonatal Resuscitation among Health Care Providers in Tertiary Care Hospitals of Nepal. Dinkum Journal of Medical Innovations, 3(03):257-270.
- Veettil S, Rajiah K, Kumar S. Study of drug utilization pattern for acute exacerbation of chronic obstructive pulmonary disease in patients attending a government hospital in Kerala, India. J Family Med Prim Care. 2014;3(3):250.
- A V A, C S, M K, Unni PVS, Salim S. A Study on Prescription Pattern and Assessment of Smoking as a Risk Factor among COPD Patients in a Tertiary Care Hospital. Indian Journal of Pharmacy Practice. 2022;15(2):90–6.
- Kumar S, Madhuri G M, Wilson A, George TS. Study of Prescribing Pattern of Drugs in Chronic Obstructive Pulmonary Disease in Tertiary Care Teaching Hospital. Indian Journal of Pharmacy Practice. 2019;12(3):161–6.
- Arya Gigi 1*, Sharon Sunil 1, Prince Hepzhiba 1, N. M. Mahesh 1, Mrudula Giri 1 AK 2. Assessment of Drug Prescribing Pattern in Chronic Obstructive Pulmonary Disease Patients at a Tertiarycare Hospital. journal of pharmacrutical research. 2015;
- Sireesha V* KB. A study on drug utilization pattern in tertiary care hospital for chronic obstructive pulmonary disease. international journal of pharmacometrices and integrated biosciences. 2018;3(1).
- M B, D B. Retrospective Study on Prescription Pattern on the Management of Chronic Obstructive Pulmonary Disease (COPD). International Journal of Advanced Multidisciplinary Research and Studies. 2024;4(2):1491–6.
- Kushwaha N. A study of prescription pattern among COPD patients in a tertiary care hospital. 2023;403–9.
- Salwan P, Singla J, Salwan S. Prescription pattern in the management of chronic obstructive pulmonary disease patients in a tertiary hospital: an observational study. Int J Basic Clin Pharmacol. 2020;9(10):1578.
- Jyothi DB, Prasad SV, Vangoori Y, Bharatha A. A Prospective Study on Prescription Pattern in Chronic Obstructive Pulmonary Disease. Maedica (Bucur). 2020;15(1):37–44.
- Sai Lakshmi Srikala T, Saika V, Raveendra Babu K, Chinna Eswaraiah M. Assessment of prescription pattern among copd patients in departments of general medicine ward and pulmonology in tertiary care hospitals of Khammam region. International Journal of Research in Pharmaceutical Sciences. 2020;11(2):1798–806.
- Shifani M, Santhiyya E, Nithyanandham K. Original Research Paper Medicine Dr. Lakshmi Sabapathi * Maria Infant Majula. 2022;(2277):28–31.
Publication History
Submitted: February 16, 2025
Accepted: March 02, 2025
Published: March 31, 2025
Identification
D-0417
DOI
https://doi.org/10.71017/djmi.4.3.d-0417
Citation
Nabin Thapa Magar, Manish Adhikari, Swagat Khadka & Mahendra Acharya (2025). Drug Utilization Pattern of COPD in KANKAI Municipal Hospital, KANKAIN Municipality, JHAPA. Dinkum Journal of Medical Innovations, 4(03):136-146.
Copyright
© 2025 The Author(s).


