Publication History
Submitted: March 20, 2025
Accepted: March 28, 2025
Published: April 30, 2025
Identification
D-0421
DOI
https://doi.org/10.71017/djmi.4.4.d-0421
Citation
Mukesh Jaiswar , Ashok Kumar Rokaya, Narad Prasad Thapaliya, Gonish Hada, Nirmal Thapa & Sudhan Subedi (2025). Comparative Clinical Study of Non-Mesh versus Mesh Repair in Primary Inguinal Hernia. Dinkum Journal of Medical Innovations, 4(04):190-208.
Copyright
© 2025 The Author(s).
190-208
Comparative Clinical Study of Non-Mesh versus Mesh Repair in Primary Inguinal HerniaOriginal Article
Mukesh Jaiswar 1 *, Ashok Kumar Rokaya 2, Narad Prasad Thapaliya 3, Gonish Hada 4, Nirmal Thapa 5, Sudhan Subedi 6
- Karnali Academy of Health Sciences, Jumla, Nepal.
- Karnali Academy of Health Sciences, Jumla, Nepal.
- Karnali Academy of Health Sciences, Jumla, Nepal.
- Nepal Medical College and Teaching Hospital, Kathmandu, Nepal.
- Karnali Academy of Health Sciences, Jumla, Nepal.
- Karnali Academy of Health Sciences, Jumla, Nepal.
* Correspondence: mukeshjaiswar1003@gmail.com
Abstract: A hernia is defined as a protrusion of a viscus through an opening in the wall of the cavity in which it is contained. Hernias of the abdominal wall occur only in areas where aponeurosis and fascia are devoid of the protecting support of striated muscle. This study compared open mesh and non-mesh suture repair of primary inguinal hernias with respect to clinical outcome which include postoperative pain, complications, time of return to work and recurrence. It had been conducted on patients admitted for primary inguinal hernia who were either repaired by non-mesh suture method using 2/0 prolene suture or by open polypropylene (Prolene) prosthetic mesh. Study was carried out on cases which included N=102 patients who underwent primary inguinal hernia repair. Of the 102 patients, 52 patients underwent non-mesh repair whereas 50 patients underwent open mesh repair. Two methods were used, non-mesh suture method and mesh suture method. In 102 cases which underwent primary hernia repair, 100 were male patients and 2 were female patients. 60% of the cases were above the age of 50 years and 60.8% were right sided and 39.2% left sided. On the basis of presenting symptoms out of 102 patients, 66 patients got Swelling in the inguinoscrotal region i.e. 64.7%, 20 patients feel pain in the inguinal region i.e. 19.6%, and 16 patients got discomfort in the inguinoscrotal region i.e. 15.7%. out of 102 patients, 62 patients are Risk factors, Prostatism, Constipation, Coughing, Diabetes, Use of steroids, Smoking, out of these risk factors coughing is more common in non-mesh and mesh repair than other risk factors. Inguinal hernia repair performed by suturing and displacement of anatomic structures may lead to excessive tension on the suture line and surrounding tissue. The use of prosthetic mesh allows tension-free repair of inguinal hernia and in theory better results.
Keywords: primary, inguinal hernia, non-mesh, mesh repair, comparative
- INTRODUCTION
The term inguinal hernia was derived from the Greek word meaning an off shoot, a budding or bulge. The Latin word hernia means a rupture or tear. Trusses and bandages generally were used to control the herniation. Celsus in the first century AD gave incisions in the neck of the scrotum, the hernial sac was dissected off the spermatic cord and transacted at the external inguinal ring. The testis was excised as well. An author, differentiated between inguinal and femoral hernia and described the technique of reduction for strangulation. A study distinguished direct from indirect hernia and advised that the testicle need not be removed [1]. An American surgeon [2] was the first to recognise the importance of transversalis fascia and of closing the internal ring. A study [3] reported the first case in which the aponeurosis of the external oblique muscles was slit to reveal the canal, which allowed dissection and ligation of the sac at the internal ring under direct vision. Results were not good then, the recurrence rate being 30% to 40% after 1 year and almost all hernias recurred by the end of 4 years. The greatest contribution to hernia surgery was that of the Italian surgeon Edoardo Bassini [1]. He laid the inguinal canal open widely by splitting the aponeurosis of the external oblique. He next opened the transversalis fascia from the pubic tubercle to beyond the internal ring, dissected and ligated the sac high in the retro peritoneal space. He repaired the transversalis fascia and re-in forced the posterior wall of the canal by suturing the internal oblique and transversalis abdominis muscle as well as the upper leaf of the transversalis fascia and the inguinal ligament using interrupted sutures of silk. The aponeurosis of the external oblique was re sutured in front of the spermatic cord. An author [4] reported an almost 100% follow up his patients for 5 years with 11 wound infections and only 8 recurrences. These phenomenal results earned him the title of “Father of Modern Herniorrhaphy”. An author first reported the technique of suturing the conjoined tendon to the pectineal ligament as opposed to the inguinal ligament [5]. A study [6] popularised this method and in 1940 showed by anatomical dissections that the transversus abdominis muscle and its fascia are normally inserted into the pectineal ligament. Critics of the pectineal ligament repair are of the opinion that since this ligament is lower down and further posterior to the inguinal ligament, a great deal more tension was brought about by bringing the conjoined tendon down to the pectineal ligament. During the next 100 years most, inguinal hernia was repaired by the Bassini method or variations of it [7]. Notable among the improvements was the multilayered repair described by [8]. Repair of the transversalis fascia and tightening of the internal ring was the basis of this tissue type of repair. After suitable exposure of the transversal is fascia and the internal ring and freeing the spermatic cord from its edges, the transversalis fascia was slit open from the medial pillar of the internal ring up to the pubic tubercle and the two flaps were raised. The first layer of the repair was by suturing the free edge of the lower flap high behind the upper flap to the posterior aspect of the transversalis fascia as well as the posterior aspect of the rectus sheath and of the aponeurosis of the transverses abdominis. 34 gauze stainless steel wire continuous suture was used. The next layer of the repair was from the lateral end suturing the free edge of the upper leaf of transversalis fascia to the base of lower edge and the iliac pubic tract and to the inguinal ligament up to the pubic tubercle. This double layer of overlapped transversalis fascia and muscle formed a new strong posterior wall of the canal. The posterior wall was further strengthened by another double layer that sutured the conjoined tendon to the inguinal ligament and lower flap of the external oblique aponeurosis [9]. The cord was now laid on these four layered buttresses and the external oblique aponeurosis was closed in front of the cord in a single or double layer. The recurrence rate in primary hernia repair as reported from the Shouldice Hospital in Toronto is <1%; However, this method is rather complicated and calls for extensive dissection and suturing under tensions [10]. A hernia is defined as a protrusion of a viscus through an opening in the wall of the cavity in which it is contained. Hernias of the abdominal wall occur only in areas where aponeurosis and fascia are devoid of the protecting support of striated muscle. Without a counteracting force, the bare aponeurotic areas are subjected to the ravages of intra- abdominal pressure and give way if they deteriorate or contain anatomical irregularities. The inguinal regions are one of the natural weak areas in the abdominal wall and are the most common site of herniation [11]. The incidence of inguinal hernia in adults varies between 10% to 15%. Hernias are present in more than 45% of males at 75 years of age and older [1]. An author classified inguinal hernia into direct and indirect hernia [1]. Inguinal hernia repair is one of the most frequently performed operations. Failure of inguinal hernia repair leads to increased patient discomfort and re-operations results in a considerable burden on the patient. Chances of hernia recurrence after open surgery ranges from 1% to 7% for an indirect hernia and from 4% to 10% for a direct hernia [2]. Though there are various reasons for the failure of repair, the method of repair plays a vital role in the success of inguinal hernia repair. Until recently the standard procedure has been open Musculo-aponeurotic repair using sutures under tension to close the defect but ‘tension- free’ repair using prosthetic mesh is becoming increasingly common in many countries. Use of Lichtenstein mesh repair increased from 33% in January 1998 to 62% in June 2000 [3]. No consensus has yet been reached about the surgical approach to inguinal hernia repair that gives best clinical result [5,6,7]. The optimal method for inguinal hernia repair is yet to be determined [5]. This study compared open mesh and non-mesh suture repair of primary inguinal hernias with respect to clinical outcome which include postoperative pain, complications, time of return to work and recurrence.
- MATERIALS & METHOD
This study had been conducted on patients admitted for primary inguinal hernia who were either repaired by non-mesh suture method using 2/0 prolene suture or by open polypropylene (Prolene) prosthetic mesh. The study was done at Medical College and Hospital. Prospective study was carried out on cases included 102 patients who underwent primary inguinal hernia repair. Of the 102 patients, 52 patients underwent non-mesh repair whereas 50 patients underwent open mesh repair. All patients older than 18 years scheduled for repair of a primary inguinal hernia were randomised to either non-mesh or mesh repair. Patients were enrolled only once. Age, Sex, intermittent high abdominal pressure i.e., persistent cough, constipation, prostatism and factors that may interfere with wound healing i.e., diabetics, use of steroids, smoking were noted. All patients were thoroughly examined, the type of inguinal hernia diagnosed clinically was noted and basic investigations were done. One hour before operation a single dose of intravenous Cefotaxime was administered. Patients underwent operation under either spinal anaesthesia with Bupivacaine or local anaesthesia consisting of 0.5% lignocaine and 0.25% bupivacaine administered by local-layer infiltration. All patients were monitored by pulse oximeter. Following inductions/infiltration of anaesthesia, the skin and subcutaneous tissue were incised and the external oblique aponeurosis was slit open completing the incision through the superficial inguinal ring. The upper leaf of external oblique was separated from the internal oblique by blunt dissection and the lower leaf was separated from the contents of the inguinal canal until the inner aspect of inguinal ligament was seen. The indirect sac was dissected free up to the deep inguinal ring and making sure it was empty the sac was opened; all the contents were reduced and the neck was transfixed as high as possible before excising the sac. The direct sac was invaginated. The re-enforcement of the posterior inguinal wall was achieved by suturing with 2/0 polypropylene suture (Prolene no 2/0, Ethicon) without tension between the tendinous aponeurotic arch of internal oblique to the under surface of the inguinal ligament. The external oblique aponeurosis then was sutured in front of the cord and the wound closed. Mesh repair was performed according to a strict protocol as described by Lichtenstein using a polypropylene prosthetic (Prolene) mesh of adequate size to avoid tension on the suture lines. Prolene mesh is made of synthetic polymer. Prolene mesh is constructed of knitted non-absorbable filaments of an isotactic crystalline stereoisomer of polypropylene; a synthetic linear polyolefin (C3 H6) n. Prolene mesh is knitted by a process which interlinks each fibre junction and which provides for extensibility in both directions. This construction permits the mesh to be cut into any desired shape or size without unravelling. The fibre junctions are not subject to the same work fatigue exhibited by more rigid metallic meshes. This bi-directional extensible property allows adaptation to various stresses encountered in the body. Prolene mesh elicits a minimal initial inflammatory reaction in tissues, which is transient and followed by deposition of a thin fibrous layer of tissue which can grow through the interstices of the mesh, thus incorporating the mesh into adjacent tissue. The material is not absorbed nor is it subjected to degradation or weakening by the action of tissue enzymes. According to [4], all available laboratory date indicated that the mesh does not degrade or deteriorate during the life time of the patient. Extended flex time of mesh has been explained by the fact that the molecules of this material are in a shape of helix.
Thickness of Mesh : 0.69 mm
Softening point of mesh : – 140° c
Melting point of mesh : – 335° c
Strength of mesh : – 17.5 kg/cm2.
The skin and subcutaneous tissue was incised and the external oblique aponeurosis was slit open completing the incision through the superficial inguinal ring. The upper leaf of external oblique was separated from the internal oblique by blunt dissection and the lower leaf was separated from the contents of the inguinal canal until the inner aspect of inguinal ligament was seen. The cord was elevated from the posterior wall of the canal. The indirect sac was dissected free and transfixed at the deep inguinal ring making sure it contained nothing and excised. The direct sac was invaginated. A sheet of polypropylene mesh measuring 8 cm x 6 cm was trimmed to fit the area exposed and used to reconstruct the entire floor of the inguinal canal without any attempt to close the defect by suture. The mesh was sutured along its lower edge to the public tubercle, the lacunar ligament and the inguinal ligament with 2/0 prolene suture. The superior edge was tacked down to the aponeurosis or muscle of the internal oblique with a few interrupted sutures. The lateral edge of the mesh was slit and the two tails passed around to embrace the cord at the deep inguinal ring; then they were crossed over each other and tacked down to the inguinal ligament with one polypropylene suture. The external oblique aponeurosis then is sutured in front of the cord. Any complaints of pain in the operated site were noted. Pain was scored daily for first 3 post operative days and in the subsequent follow up visits on a four-point verbal rank scale: no pain, light pain, moderate pain or severe pain. On the second postoperative day, the operated site was looked for any wound hematoma, seroma or wound infection and if found healthy the patient was discharged on the 3rd post operative day. The patient was followed up on 7th post operative day when the stitches were removed. Subsequently the cases were followed up at 1,6,12, 24 months. Awareness of hernia recurrence and complaints about the groin were noted and the groin was examined physically.
- RESULTS & DISCUSSION
Table 01: Age of the participant of the study
| Age group (in years) | No. of cases | % of cases |
| 18 – 30 | 5 | 4.9 |
| 31 – 40 | 13 | 12.7 |
| 41 – 50 | 23 | 22.5 |
| 51 – 60 | 22 | 21.5 |
| 61 – 70 | 25 | 24.5 |
| 71 – 80 | 14 | 13.7 |
60% of the cases are >50 years of age. In 102 cases who underwent primary hernia repair, 100 were male patients and 2 were female patients. 60% of the cases were above the age of 50 years and 60.8% were right sided and 39.2% left sided.
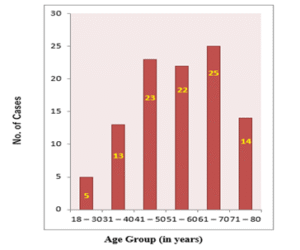
Figure 01: Age Group
Table 02: Gender of the participants
| Male | Female |
| 100 | 2 |
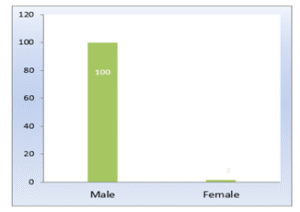
Figure 02: Out of 102 patients,100 patients are male and 2 patients are female, which is shows that male more suffer than female.
Table 03: Presenting symptoms of the participants
| Symptoms | No. of cases | % |
| Swelling in the inguinoscrotal region | 66 | 64.7 |
| Pain in the inguinal region | 20 | 19.6 |
| Discomfort in the inguinoscrotal region | 16 | 15.7 |
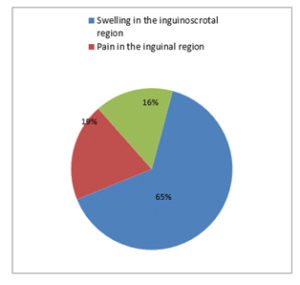
Figure 03: Presenting Symptoms
Table 04: Sides of the cases
| Side | No. of cases | % |
| Right | 62 | 60.8 |
| Left | 40 | 39.2 |
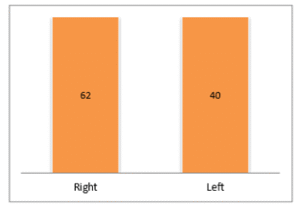
Figure 04: Side
Table 05: Risk factors of mesh and non-mesh cases
| Risk factors | Mesh | Non-mesh |
| Prostatism | 15 of 48 | 8 of 52 |
| Constipation | 6 of 50 | 10 of 52 |
| Coughing | 18 of 50 | 11 of 52 |
| Diabetes | 4 of 50 | 6 of 52 |
| Use of steroids | 0 of 50 | 0 of 52 |
| Smoking | 12 of 50 | 10 of 52 |
Table 06: Type of hernia on clinical examination
| Type of hernia | No. of cases | % |
| INDIRECT | 64 | 62.7 |
| Inguinal | 54 | 84.4 |
| Inguinoscrotal | 10 | 15.6 |
| DIRECT | 38 | 37.3 |
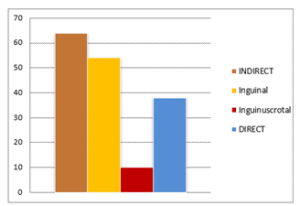
Figure 05: Type of hernia on clinical examination
Table 07: Type of anaesthesia
| Type of anaesthesia | No. of cases | % |
| Local anaesthesia | 18 | 17.6 |
| Spinal anaesthesia | 84 | 82.4 |
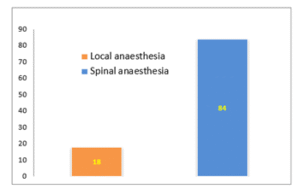
Figure 06: Type of Anesthesia
Table 08: Type of hernia on operation according to Gilbert classification
| Type | No. of cases | % |
| Type 1 | 3 | 2.9 |
| Type 2 | 49 | 48 |
| Type 3 | 3 | 2.9 |
| Type 4 | 37 | 36.3 |
| Type 5 | 0 | 0 |
| Type 6 | 10 | 9.8 |
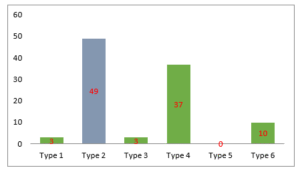
Figure 07: Type of hernia on operation according to Gilbert classification
Table 09: Operative procedure
| Type of procedure | No. of cases | % |
| Mesh repair | 50 | 49 |
| Non-mesh repair | 52 | 51 |
In 102 patients 52 patients randomly underwent non-mesh repair and 50 patients underwent mesh repair.
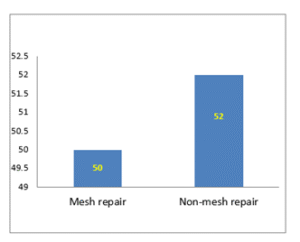
Figure 07: Operational Procedures
Table 10: Time taken in minutes
| Time taken | Average (minutes) | Range (minutes) |
| Mesh repair | 40 | 30 – 90 |
| Non-mesh repair | 45 | 40 – 90 |
Median duration of Surgery for non-mesh repair was 40 minutes (range 30 – 90 minutes) and for mesh repair was 45 minutes (range 40 – 90 minutes).
Table 11: Post operative pain non-mesh repair
| Verbal rank | No. of cases | % |
| No pain | 8 | 15.4 |
| Light pain | 30 | 57.7 |
| Moderate pain | 10 | 19.2 |
| Severe pain | 4 | 7.7 |
Light pain post operative pain in non-mesh repair is 57.7%, moderate pain is 19.2%, severe pain is 7.7% and no pain is 15.4%.
Table 12: Mesh repair
| Verbal rank | No. of cases | % |
| No pain | 13 | 26 |
| Light pain | 33 | 66 |
| Moderate pain | 2 | 4 |
| Severe pain | 2 | 4 |
No pain in mesh repair is 26%, light pain is 66%, moderate pain is 4% and severe pain is 4%.
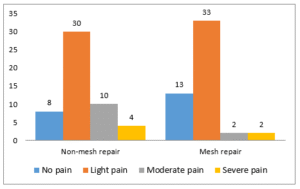
Figure 09: Repair
60% of the patient experienced persisting pain and had to be given oral Diclofenac 50mg daily for 5 days. Intensity of pain was less in the mesh repair group and 20% of the patients experienced persisting pain.
Table 13: Hospital stays
| Method | Median (days) | Range (days) |
| Non-mesh | 5 | 2 – 10 |
| Mesh | 3 | 1 – 5 |
The median hospital stay was 5 days (range 2 – 10 days) for non-mesh repair group and 3 days (range 1 – 5 days) for mesh repair group.
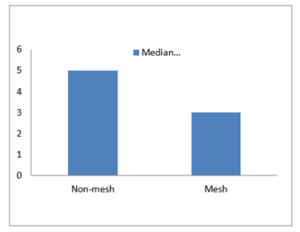
Figure 10: Hospital Stay
Table 14: Time off work
| Method | Median (days) | Range (days) |
| Non-mesh | 21 | 7 – 45 |
| Mesh | 19 | 7 – 30 |
Time off work was 21 days (range 7–45 days) for non-mesh repair group and 19 days (range 7–30 days) for mesh repair group.
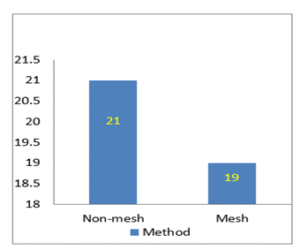
Figure 11: Time of Work
Table 15: Complications Wound infection
| Method | No. of cases | % | |||
| Mesh | 1 | 2 | |||
| Non-mesh | 3 | 5.76 | |||
| Non-mesh | 3 | 5.76 | |||
1 case (2%) of mesh repair group had a localized stitch abscess which subsided following intravenous Cefotaxime for 5 days. In the non-mesh repair group 3 cases (5.7%).
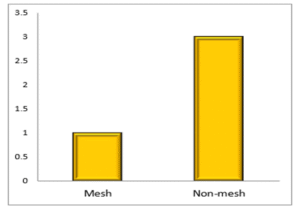
Figure 12: Wound Infection
Table 16: Hematoma
| Method | No. of cases | % |
| Mesh | 0 | 0 |
| Non-mesh | 2 | 3.8 |
Hematoma occurred in 2 cases (3.8%) of non-mesh group and not noted in any case of mesh repair group.
Table 17: Seroma
| Method | No. of cases | % |
| Mesh | 0 | 0 |
| Non-mesh | 4 | 7.7 |
Seroma was noted in 4 cases (7.7%) of non-mesh repair group and not noted in any case of mesh repair group.
Table 18: Recurrence
| Follow up period | Non mesh repair | Mesh repair |
| 0 – 1 month | 0 | 0 |
| 1 – 6 months | 0 | 0 |
| 6 – 12 months | 1 | 0 |
| 1 – 2 years | 0 | 0 |
1.9% recurrence following non-mesh repair.
During the 2 years follow up 1 case (1.9%) recurrence was found in the non-mesh repair group and none in the mesh repair group.
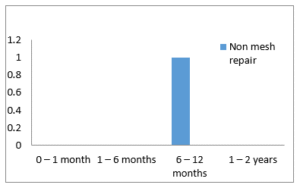
Figure 13: Recurrence
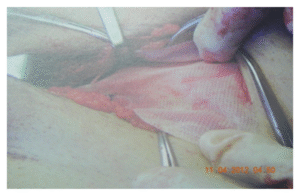
Figure 14: With Mesh Repair Hernia (lt. side)
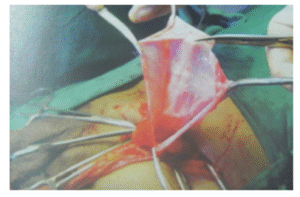
Figure 15: With Non-Mesh Repair Hernia (lt. side)
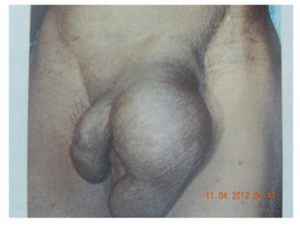


Figure 16: Inguinal Hernia (lt. side)
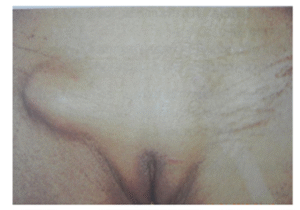
Figure 17: Female Inguinal Hernia (rt. side)
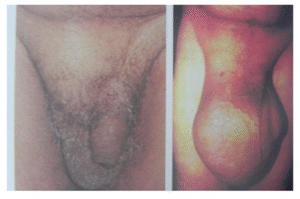
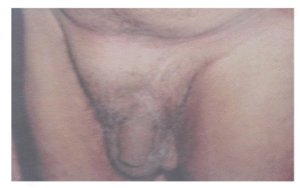
Figure 18: Inguinal Hernia (rt. side)
DISCUSSION
In our prospective study of 102 cases underwent primary hernia repair, 100 were male patients and 2 were female patients. 60% of the cases were above the age of 50 years and 60% were right sided. 18 cases randomly received local anaesthesia whereas 84 cases received spinal anaesthesia. No cases of urinary retention were found in those who received local anaesthesia but 26 cases (30%) of those who received spinal anaesthesia developed urinary retention in the postoperative period and had to be catheterised. Early ambulation soon after operation was also possible in the cases who received local anaesthesia. In the study of 3175 primary inguinal hernia repairs using polypropylene mesh under local anaesthesia had no cases of urinary retention [12]. All open hernia techniques lend themselves ideally to local anaesthesia. Open mesh repair under local anaesthesia is an effective day care technique particularly in the elderly and medically unfit. Median duration of Surgery for non-mesh repair was 40 minutes (range 30 – 90 minutes) and for mesh repair was 45 minutes (range 40 – 90 minutes). An author [13] reported that operative time for mesh repair (111+/-2 minutes) was longer than for Bassini or MC Vay (91+/- 2 and 98+/- 2 minutes). In our study there was no specific criteria for allocation of the method of repair and of 102 patients 52 patients randomly underwent non-mesh repair and 50 patients underwent mesh repair. Both groups experienced pain in the postoperative period. The intensity of pain at 24 hours, 48 hours and 7 days after surgery was greater in the non-mesh repair group. 60% of the patient experienced persisting pain and had to be given oral Diclofenac 50mg daily for 5 days. Intensity of pain was less in the mesh repair group and 20% of the patients experienced persisting pain. As reported by [14]; mesh repair appeared to reduce the chance of persisting pain rather than increasing it. However [15], had reported that choice of surgical technique for open repair of a primary inguinal hernia has no influence on post operative pain. Neuropraxia and hypesthesia have been reported in 15% to 20% of patients following open hernia repair, whereas chronic pain was seen in 5% cases [16]. In our study median hospital stay was 5 days (range 2 – 10 days) for non-mesh repair group and 3 days (range 1 – 5 days) for mesh repair group. An author [17] reported in 2002 that hospital stay in non-mesh repair cases was 4.2 days as compared to 1.8 days in mesh repair cases in primary inguinal hernia. Time off work was 21 days (range 7–45 days) for non-mesh repair group and 19 days (range 7–30 days) for mesh repair group. It was found perhaps not surprisingly that manual workers took slightly longer (median of 30 days) than did desk workers or retirees (median of 20 days) to return to normal routine. An author [18] reported in their study that return to work for non-mesh repair cases was 17.2 days as compared to 7.3 days in mesh repair cases in primary inguinal hernia. Post operative wound infection is one of the most serious complications of repair of groin hernias. In our study 1 case (2%) of mesh repair group had a localized stitch abscess which subsided following intravenous Cefotaxime for 5 days. In the non-mesh repair group 3 cases (5.7%) had acute cellulites around the wound with pus discharge from the open wound. The phase settled down following intravenous Cefotaxime and regular dressing and the wound healed. All these patients who had wound infections were of the elderly age group. It has been reported that older patients specifically over 70 years of age show a 3.2-fold higher incidence of wound infections [19]. An author [20] in his study of 892 patients reported 1% infection in those who had mesh repair and 1.8% in those who had non-mesh repair. Hematoma occurred in 2 cases (3.8%) of non-mesh group while subsided after aspiration whereas it was not noted in any case of mesh repair group. Seroma was noted in 4 cases (7.7%) of non-mesh repair group. An author [21] reported that there were no clear differences between mesh and non-mesh groups for hematomas, seromas or wound infections. During the 2 years follow up 1 case (1.9%) recurrence was found in the non-mesh repair group and none in the mesh repair group. The case which recurred was male and more than 70 years of age. The recurrence was noted during the first year of postoperative period. The case didn’t have any postoperative complication. Though 50% of recurrences are caused by infection, in our study infection was not associated with recurrence. The case was non-smoker and didn’t have any co-morbid conditions like chronic cough or prostatism. A higher percentage of smoker develops recurrences after repair as systemic protease/antiprotease imbalance in them leads to fascial degeneration and interference with normal wound healing. Abramson and colleagues showed that chronic cough was not associated with recurrence. As such prostatic hypertrophy is of no significance in the development of a hernia or recurrence after repair [22]. The approximation of tissues under tension is a cardinal factor in the failure of a hernia repair. Tissues sutured under tension tend to pull apart but are prevented from doing so by the sutures; however, the tissue pulling on the sutures create an area of ischemic pressure necrosis where the suture meets the tissue. This process of ischemic necrosis progresses until there is no longer any tension, which usually occurs when the tissues have returned to their previous un sutured position and the hernia recurs through the resultant gap. In more extreme cases in which the tension is greater than the strength of the tissues, the sutures simply tear the tissues and the hernia recurs. A study [23] compared the Shouldice technique and Lichtenstein tension free mesh technique in 178 patients operated upon by trainees. Duration of operation and complication rates was similar. Mesh repair resulted in less days of sick leave (18 versus 23 days, p<0.05) and fewer recurrences (nil versus 9, p<0.01). He concluded that for surgeons in training the Lichtenstein open mesh technique is a better method of inguinal hernia repair than the Shouldice technique. “Comparison of non-mesh (Desarda) and mesh (Lichtenstein) methods for inguinal hernia repair among black African patients and the best result shows in mesh repair hernia. Study was done for 150 patient and in the study population 70 patient were subjected to non-mesh (Desarda) and the rest underwent mesh (Lichtenstein) methods [24,25]. A study [26] reviewed 21 trials comparing open mesh with open non-mesh repair in primary inguinal hernia. Open mesh methods on average took 7–10 minutes less to perform than Shouldice procedures but took 1–4 minutes longer than other non-mesh methods. Those in the mesh groups had a shorter length of hospital stay and quicker return to usual activities. They concluded that the use of open mesh repair is associated with a reduction in the risk of recurrence between 50% and 75%. An author [27] did a study to compare mesh versus non-mesh inguinal herniorrhaphy. From 1985 to 1994 892 patients underwent primary repair for inguinal hernia at the Veteran’s Administration Hospital at Memphis, TN. Mesh patients developed four wound infections (1.0%) none requiring mesh removal versus nine infections (1.8%) in non-mesh repair. One mesh patient (0.3%) developed recurrence compared with 16 (3.5%) with open anterior repair (p<0.01). In a study done by [28], 62 relevant comparisons were made in 58 trials. These included 11,174 patients. Recurrence and persisting pain were less after mesh repair. In a systematic review of randomized controlled trials carried out by [29], in was reported that return to usual activities was quicker in the mesh group. There were fewer recurrences in the mesh group; 21 (1.4%) of 1513 versus 72 (4.4%) of 1634 (p<0.001). An author [30] did a prospective study of 26,304 groin hernia repair in Denmark between Jan 1, 1998 to Jan 30, 2000 and reported that reoperation rates 30 months after anterior mesh repair and laparoscopic repair were significantly lower than after sutured posterior wall repair in primary inguinal hernia (2.2% and 2.6% vs 4.4%; p<0.0001). Use of Lichtenstein mesh repair increased from 33% in January 1998 to 62% in June 2000 whereas use of laparoscopic repair remained constant at about 5%. Reoperation rates were 2.8% in the first 15 months and 1.6% in the second. A retrospective comparison of 182 on lay mesh repairs and 170 Bassini repairs carried out by surgeons in training found five recurrences (3.3%) in the mesh repair group and 13 (11.5%) in the Bassini group [31]. A review of literature on the results of herniorrhaphies reveals that for inguinal repair, recurrence was as follows:
Bassini : recurrence, 2.9% to 25.0%
Shouldice : recurrence, 0.2% to 2.7%
McVay : recurrence, 1.5% to 15.5%
Nyhus : recurrence, 3.2% to 21%
For operations using mesh, the recurrence rates were as follows:
Lichtenstein’s Tension free repair: recurrence, 0% to 1.7%
Nyhus Buttress : recurrence, 0% to 1.7%
Rives : recurrence, 0% to 9.9%
Stoppa : recurrence, 0% to 7%
Plug repair : recurrence, 0% to 1.6%
For laparoscopic repairs [32]:
IPOM : recurrence, 0% to 4.5%
TAPP : recurrence, 1% to 4.3%
TEP : recurrence, 0% to 0.4
- CONCLUSION
The prospective study of 102 cases of primary inguinal hernia repair conducted at Sichuan Medical University compared mesh and non-mesh suture repair with respect to clinical outcomes, including postoperative pain, complications, duration of hospital stay, time to return to work, and recurrence rates. The majority of patients were older than 50 years, with males outnumbering females, and 64.7% presenting with inguinoscrotal swelling. Right-sided (60.8%) and indirect hernias (62.7%) were most common. No cases of urinary retention were noted among patients who underwent repair under local anesthesia. Operative time was longer for mesh repair than for non-mesh repair; however, postoperative pain was less in the mesh repair group. Hospital stay was shorter for mesh repair (median: 3 days) compared to non-mesh repair (median: 5 days). Similarly, return to work was earlier in mesh repair patients (19 days) than in non-mesh repair patients (21 days). The overall complication rate was lower in the mesh repair group, with reduced incidence of wound infection (2% vs. 5.7%), hematoma (0% vs. 3.8%), and seroma formation (0% vs. 7.7%). At two years of follow-up, no recurrences were observed in the mesh group, whereas one recurrence (1.9%) occurred in the non-mesh group during the first postoperative year, independent of chronic cough, prostatism, or infection. These findings highlight that suture-based repairs, which displace anatomic structures and generate excessive tension on the suture line, are more prone to recurrence and complications. In contrast, prosthetic mesh provides a tension-free repair with better long-term outcomes. The results of the study confirmed the superiority of mesh repair over non-mesh repair in terms of reduced pain, fewer complications, shorter hospitalization, earlier return to work, and significantly lower recurrence rates. Therefore, mesh repair should be regarded as the method of choice for primary inguinal hernia repair.
REFERENCES
- Jack Abrahamson. Hernias. Maingot’s Abdominal Operation Vol 1 2001; 479-525.
- Scott DJ, Jones DB (2000). Hernias And Abdominal Wall Defects. In JA Norton Et Al, Eds., Surgery: Basic Science And Clinical Evidence, PP 803-810 New York: Springer.
- Aubay- Nielson M. Kehlet H. Strand L. Malmstrom J. Anderson Wara P. Juul P. Callesen T. Danish Hernia Database Collaboration T1 Quality Assessment Of 26, 304 Herniorhapheis In Denmark: A Prospective Nation Wide Study SO Lancet. 358 (9288): 11 24-8,2001 October 6.
- Bikram Duwal, Dr. Biraj Singh Karki, Dr. Lok Bahadur Kathayat & Dr. Dishan Maharjan (2024). A Study on Gallbladder Retrieval via Epigastria V/S Supraumbilical port in Laparoscopic Cholecystectomy. Dinkum Journal of Medical Innovations, 3(06):424-433..
- AV Vrijland WW. Van Den Tol MP. Luijendijk RW. Hop WC. Busschbach JJ. De Large DC. Van Geldane D. Rottier AB. Vegt PA. Ijzermans JN. Jeekel J. Randomised Clinical Trial Of Non Mesh Versus Mesh Repair Of Primary Inguinal Hernia; British Journal Of Surgery.89(3): 293-7, 2002 March.
- Mcgillicuddy JE. Prospective Randomised Comparison Of The Shouldice And Lichtenstein Hernia Repair Procedures. Arch Surg 1988; 133: 974-8.
- Barth RJ Jr, Burchard KW, Tosteson A, Sutton JE Jr, Colacchio TA, Henriques HF Et Al. Short Term Outcome After Mesh Or Shouldiceherniorrhaphy: A Randomised, Prospective Study. Surgery 1998; 123: 121-6.
- Lichtenstein PL, Shulman AG, Amid PK, Et Al: The Tension Free Hernioplasty. Am J. Surg 157: 188-193, 1989.
- Nimra Naseem, Rubab Zahra, Umm-e-Aimen & Tahir Rana (2023). Literature Review on Comparison of the effect of Single Oral Dose 150 Mg Pregabalin Premedication to Single Oral Dose 100mg Tramadol in Elective Inguinal Hernia Surgery. Dinkum Journal of Medical Innovations, 2(01):01-11.
- Rodrigues- Junior AJ, De- Tolosa EM, De Carnalho CA. Electron Microscopic Study An The Elastic And Elastic Related Fibres Fin The Human Fascia Transversalis At Different Ages. Gegenbaursmorpholjahrb 1990; 136: 645.
- Mcvay CB, Hlver4son K. Preperitonealhernioplasty. In: Beahrs OH, Beart RW Jr (Eds) General Surgery Therapy. New York, NY: John Wiley And Sons; 1981:10.
- Shouldice EE. The Treatment Of Hernia. Ontario Med Rev 1953; 20: 670.
- Welsh DRJ, Alexander MAJ. Theshouldice Repair. Surgclin North Am 1993; 73: 451.
- Mair GB. Preliminary Report On The Use Of Whole Skin Grafts As A Substitute For Fascial Sutures In The Treatment Of Hernia. Br J Surg 1945; 32: 381.
- Chitrasen Yadav, Prof. Pradeep Vaidya, Dr. Laligen Awale, Dr. Geha Raj Dahal, Sanjeeb Jha & Krishna Yadav (2024). Evaluation of Surgical Site Infections and Patterns of Microorganisms involved in Emergency Laparotomy in TUTH . Dinkum Journal of Medical Innovations, 3(08):557-569.
- Moloney GE. Results Of Nylon Darn Repairs Of Hernia. Lancet 1958; 1: 273.
- Asbin Bandhari, Syeda Hajra Batool, Aatiqa Tariq, Abdullah Hassan, Pooja Bhanarjee & Parshu Ram (2023). A Comprehensive Analysis of Neurosurgeons’ Conversations to Preserve Non-Traditional Brain Networks. Dinkum Journal of Medical Innovations, 2(06):207-216.
- Abrahamson J, Elder S: The Nylon Darn Repair For Primary And Recurrent Inguinal Hernia. Contemporary Surg 32: 33, 1988.
- Beets GL, Oosterhuis KJ, GOPM, Long Term Follow Up (12-15 Years) Of A Randomised Controlled Trial Comparing Bassini- Stettan, Shouldice, And High Ligation With Narrowing Of The Internal Ring For Primary Inguinal Hernia Repair. J Am Collsurg 1997; 185: 352-7.
- AU Nathan JD. Pappas TN. Inguinal Hernia: All Old Condition With New Solutions: Annals Of Surgery. 238: 5148-57 2003 December.
- James R. Debord. The Historical Development Of Prosthetics Is Hernia Surgery. Surg Clinic Of North America December 1998; 78: 998-999.
- Hamer- Hodges DW, Scott NB: Replacement Of An Abdominal Wall Defect Using Expanded PTFE Sheet (Gore-Tex). J Roy Collsurgedinb 30: 65, 1985.
- Gilbert AI: Inguinal Hernia Repair: Biomaterials And Suture Less Repair. Perspect Gen Surg 2: 113, 1991.
- Gilbert AI: An Anatomic And Functional Classification For The Diagnosis And Treatment Of Inguinal Hernia. Am J Surg 157: 331, 1989.
- Lichtenstein IL, Shulman AG, Amid PK, Et Al: The Lichtenstein Open “Tension-Free” Mesh Repair Of Inguinal Hernias; Surgery Today 25(7): 619-25,1995.
- AU Amid PK, Lichtenstein IL. The Lichtenstein Open “Tension-Free” Mesh Repair Of Inguinal Hernias. Rozhledy V Chisurggii. 74(6): 296-301.1995 September.
- AU Shulman AG. Amid PK. Lichtenstein IL. The Safety Of Mesh Repair For Primary Inguinal Hernias: Results Of 3019 Operations From Five Diverse Surgical Sources. America Surgeon: 58(4): 255-7, 1992 April.
- AU Mccormack K. Scott NW. GOPM. Ross S, Grant AM, EU Hernia Trialists Collaboration; Laparoscopic Techniques Versus Open Techniques For Inguinal Hernia Repair: Cochrane Database Of Systematic Reviews(1): Cdoo1785, 2003.
- AU Kark AE, Kurzer MN, Belsham PA; Three Thousand One Hundred Seventy Five Primary Inguinal Hernia Repairs: Advantages Of Ambulatory Open Mesh Repair Using Local Anaesthesia; Journal Of The American College Of Surgeons. 186(4): 447-55; Discussions 456, April 1998.
- Bendavid: Complications Of Groin Hernia Surgery; Surg Clinic Of North America December 1998; 78: 1089-1100.
- AU Scott NW, Mccormack K, Graham P, GOPM, Ross SJ, Grant AM: Open Mesh Versus Non- Mesh For Repair Of Femoral And Inguinal Hernias; Cochrane Database Of Systematic Reviews.(4): CD002197,2002.
- Jack Abraham Son: Etiology And Pathophysiology Of Primary And Recurrent Groin Hernia Formation; Surg Clinic Of North America; December 1998: 78: 953-971.
Publication History
Submitted: March 20, 2025
Accepted: March 28, 2025
Published: April 30, 2025
Identification
D-0421
DOI
https://doi.org/10.71017/djmi.4.4.d-0421
Citation
Mukesh Jaiswar , Ashok Kumar Rokaya, Narad Prasad Thapaliya, Gonish Hada, Nirmal Thapa & Sudhan Subedi (2025). Comparative Clinical Study of Non-Mesh versus Mesh Repair in Primary Inguinal Hernia. Dinkum Journal of Medical Innovations, 4(04):190-208.
Copyright
© 2025 The Author(s).


